-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
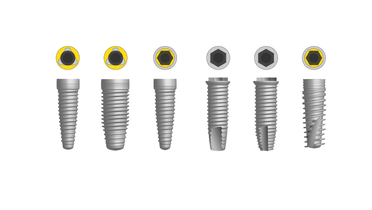
Implant placement - maxilla
Key points
- Limited risk for damaging anatomically relevant structures
- Four implants are already sufficient if proper bone quantity and quality and anterior – posterior spread of implants can be guaranteed
- Choice between fixed prosthesis and removable overdenture relate to patient age and dexterity, preference, esthetics and antero-posterior intermaxillary relation
- Esthetic outcome is often a major concern if the patient has a high lip line
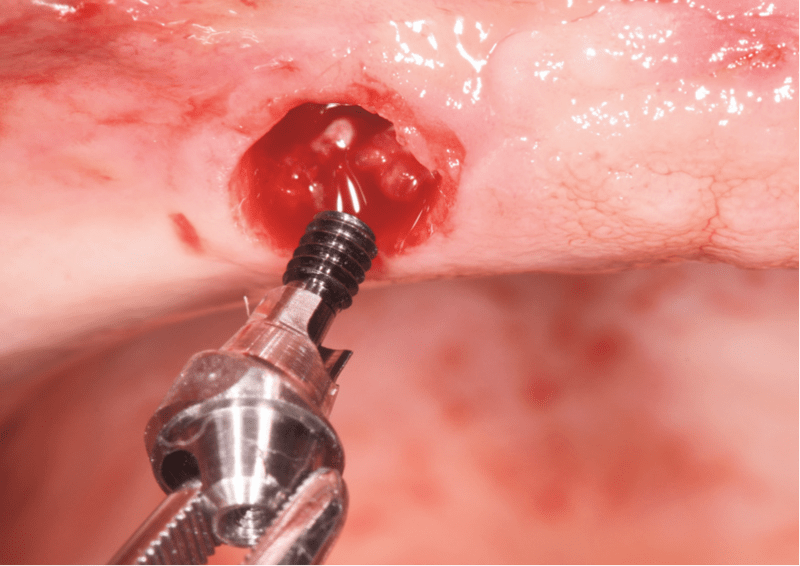
Incision
Incision can be made either on top of the crest or at some distance in the labial fold. The outcome for both approaches seems comparable. A sagittal release incision at the midline eases the reflection of the labial mucoperiosteum. It is logical to try to achieve presence of keratinized tissue both labially and palatally of the implants.
Cutting the naso-palatine neurovascular bundles rarely makes patients aware of the resulting numbness of the palatal mucosa. It often resolves after a few weeks. When maxillary bone volume is limited several authors empty and graft the naso-palatine duct with autogenous bone. Results are positive. Implants are rarely placed so posteriorly that the palatine neurovascular bundle is reached.
Primary stability considerations
If the bone is poorly mineralized, undersizing the drilled holes can nevertheless achieve a good primary stability. Primary stability assessed by measuring the implant insertion torque and/or Periotest and/or Resonance Frequency Analysis (RFA) can lead to opt for immediate or delayed loading. Using implants with turned surfaces previously led to respect a healing period of 6 months in the maxilla.
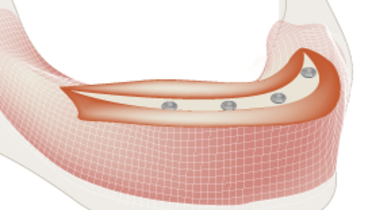
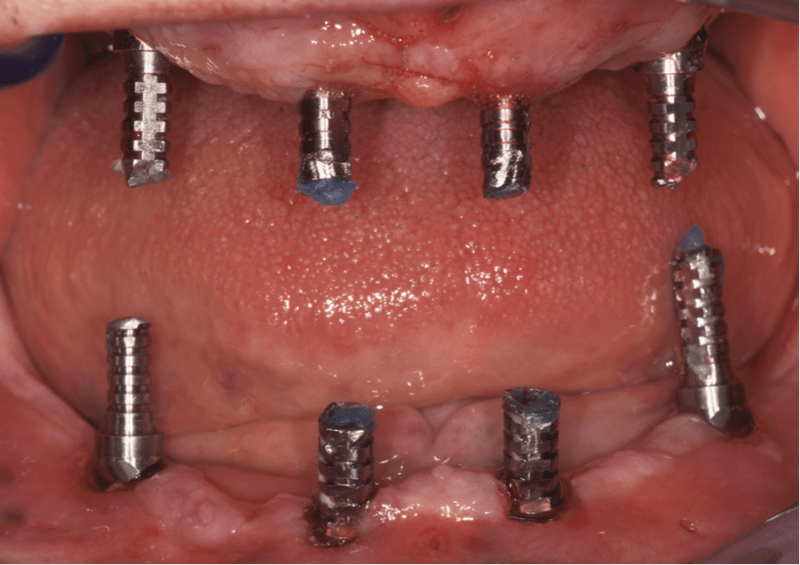
Anterio-posterior spread and implant inclination
Biomechanically it is better to reach a large anterio-posterior spread. The distal implants may be tilted dorsally, parallel to the anterior maxillary sinus wall. In the latter case, angulated abutments provide an optimal prosthetic screw access.
Also when labial inclination of the resorbed maxilla leads to an anterior tilting of the implants this can be compensated by multiunit abutments, achieving a proper parallelism (see picture). The survival rate of such tilted implants is similar to axially-oriented ones.
Fenestration of implants in the frontal region is common and does not seem to cause problems.
Number of implants and type of restoration considerations
When the patient has a high lip line and a fixed prosthesis is the treatment option, it helps to concentrate implants in dorsal areas, to provide more freedom in the front region to the dentist in charge of the prosthetic rehabilitation.
There is no consensus on the optimal number of implants needed to support a fixed complete prosthesis in the maxilla: 4 implants already provide a high predictability. In average clinicians tend to place 6 implants. Advanced maxillary bone resorption may necessitate nasal floor or sinus augmentation.
When patients cannot afford a fixed prosthesis, when the intermaxillary relation is class III or whenever there is a lack of sufficient bone volume to harbor the number of implants needed in the appropriate locations, bar-retained overdentures are preferred. If the maxillary resorption is moderate, unsplinted implants provide a favorable outcome.