-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
Hard tissue management - maxilla
Key points
- Narrow ridges are often the limiting factor for implant placement
- The ventral extension of the maxillary sinus can cause other limitations to implant placement
- Unless the use of 4 implants only to support a fixed prosthesis or overdenture does not seem predictable, invasive bone augmentation should not be considered
Bone height and width evaluation
3-D imaging seems the best option unless clinical examination reveals an ample bone volume. The bone quality can be derived from density measurements if CT scan images are available or approximately from the trabecular pattern of 2-D images. Panoramic radiographs reveal the morphology of the sinuses. Tuberosities, although often presenting with poor bone quality, can offer a site for implant insertion.
Treatment options for vertical and horizontal deficiency
If the available bone volume does not allow for implant placement, (autologous) onlay grafts have proven to offer a reliable outcome. Those can be fixed by means of implants. The invasiveness of the procedure should be considered towards the benefits and discussed with the patient.
Sacrificing of the incisal nerve does not seem to cause major symptoms and can provide a solution in some patients with very limited bone volume.
In the dorsal areas sinus inlay procedures or elevation of the mucosal lining offer reliable outcomes.
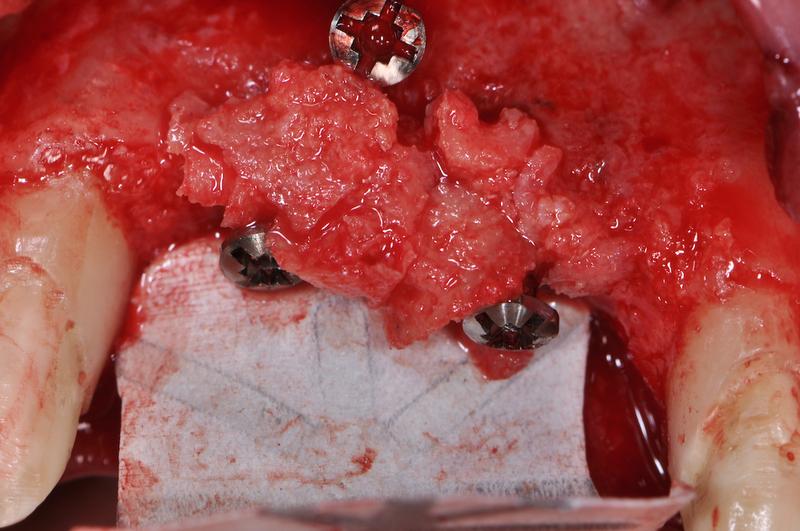
Splitting of the alveolar crest to allow for implant insertion has been proposed but the clinical documentation remains limited.





