-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
Submerged or non-submerged
Key points
- Osseointegration is a prerequisite for long term clinical success of implants
- Minimal inflammation and movement of implants are critical to osseointegration
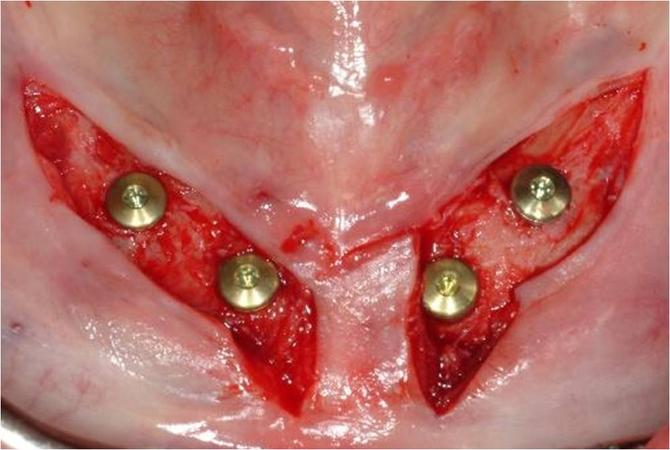
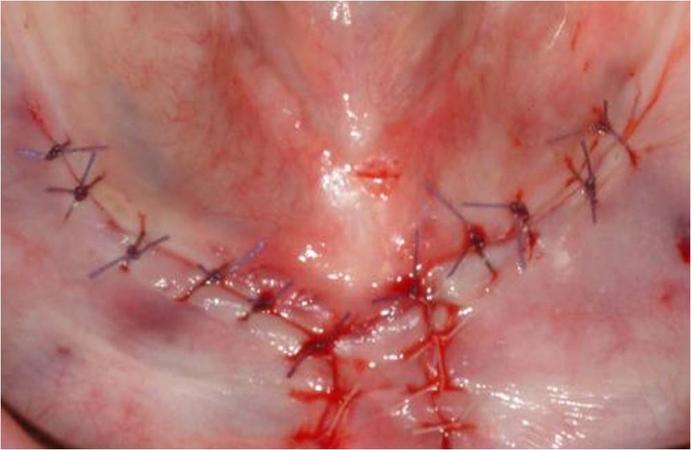
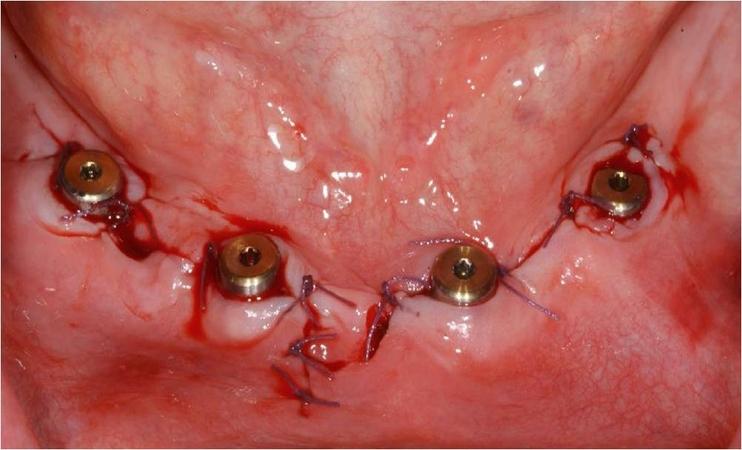
- Submerged implant healing requires a second surgical approach
Implant insertion modalities
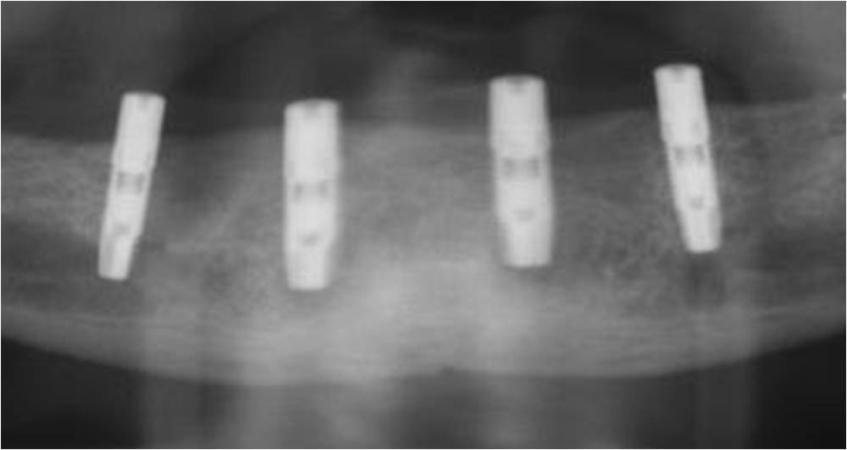
Two modalities of implant insertion are possible (Fig 1): Submerged implant insertion and non-submerged implant insertion

Implant integration into the jaw bone and surgical principles
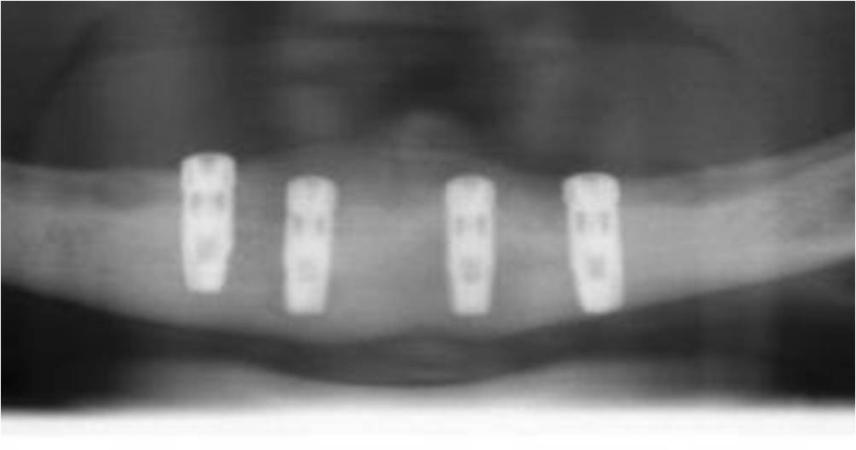
Oral endosseous implants are successful even longterm in the edentulous jaws. After insertion implants osseointegrate. This process is characterized by the development of an intimate bone contact with the implant surface. The direct anchoring of bone to the implant predicts the clinical success of the implant. Inflammation of periimplant tissues and/or movement of the implant impair the osseointegration process. To minimize the risk of impaired osseointegration historically it has been recommended to insert the implant into the bone (submerged implant) and to allow for submerged healing for 3 months in the lower jaw (Fig 1&2). After that time, during a second surgery, the implants are uncovered (Fig 2 a-c).
Subsequent clinical studies have shown that the use of non-submerged implants reached similar long-term success as submerged ones.
The treatment concept of non-submerged implant placement enables the possibility of early implant loading and a reduced treatment period for the patients (Fig 3 a-b, Table 1).
Submerged implant placement is still advocated in conditions of compromised bone quality which does not allow a sufficient primary stability at insertion, and increased risk of inflammation (like in irradiated jaw bone, or after augmentation procedures (Table 1).