-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
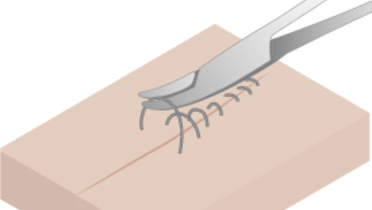
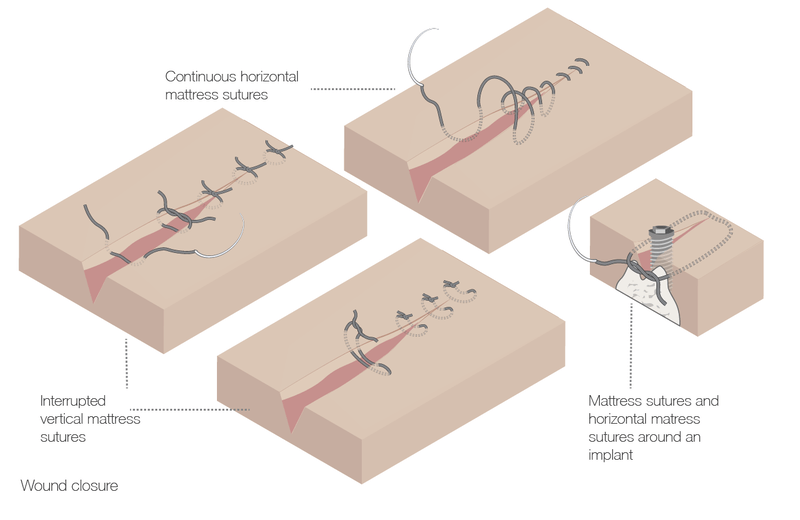
Wound closure
Key points
- Gentle tissue handling is essential for scar-free healing
- Mattress sutures are needed when wound tension is anticipated
- Monofilaments cause less mucosal inflammation but are also less comfortable for the patient
Considerations
Wound closure ensures and accelerates wound healing by protecting the site and influencing migration of keratinocytes over the granulation tissue. Some wound eversion maximizes epidermal approximation. Square knots, with two ties in one direction and a reverse direction tie as a third tie are the most commonly used types of suture. In general, interrupted sutures offer greater tensile strength than running sutures.
Technique overview
- Use of a triangular reverse cutting needle reduces risk of the suture pulling through the tissue
- Penetrate mucosa perpendicularly, i.e. at an angle of 90° to the mucosa
- Stabilize the needle with a forceps at exit prior to releasing it from the needle holder
- Gentle handling avoids tissue ischemia
- Sutures should be removed after 7-14 days, depending on the length of the wound, tension and patient age
- Delayed removal of sutures is indicated when there was high mucosal tension at the time of mattress suture placement
- Oral mucosa takes more time to heal in women than in men
- Buried resorbable sutures can be left in place
Suture and adhesive materials
- Catgut sutures should not be used any more and have been replaced by synthetic materials that present with improved properties
- Polyglycolic acid (PGA) sutures are not affected by low pH. Synthetic sutures are removed by hydrolysis, natural ones by inflammatory reaction
- Silk is less expensive than synthetic materials
- Multifilament sutures favor the migration of bacteria into the tissues
- Monofilament alternatives: polyethylene, polyester, polypropylene or expanded polytetrafluoroethylene (e-PTFE). These alternatives are more rigid and induce a reduced inflamatory response, but they are less comfortable for the patient
- Cyanoacrylate adhesives may be indicated to cover mucosal donor sites
- Fibrin-based adhesives hardly have any indication anymore in oral surgery
Clinical topics
Related articles
Questions
Ask a question
Log in or sign up to continue
You have reached the limit of content accessible without log in or this content requires log in. Log in or sign up now to get unlimited access to all FOR online resources.
No payments necessary - FOR is completely free of charge.