-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
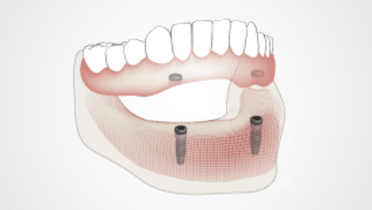
- 2.3 Implant prosthetics - removable
-
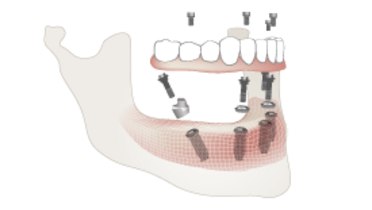
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
Mucosally supported removable - complete denture
Key points
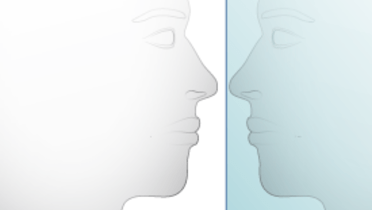
- In comparison to natural teeth, edentulous alveolar ridges offer compromised qualitative and quantitative support, that is vulnerable to residual ridge reduction (RRR)
- Denture-bearing mucosa, submucosa and underlying alveolar bone support are limited in their time dependant adaptive ability and tolerance to denture movements
- Denture looseness can lead to functional compromises (speech, chewing) and diverse clinical responses, such as denture stomatitis, Candida infection, irritation hyperplasia, ‘flabby’ ridges etc.
- For patients who do not enjoy an acceptable quality of life with complete dentures, oral implant therapy should be seriously considered
Treatment with complete dentures
Research and clinical experience show that conventional complete dentures are acceptable for a large segment of the edentulous population. Satisfied complete denture wearers are well adapted to their prosthodontic experience and have learned to eat and speak with their dentures. It is believed that the best prognosis for a denture wearing experience includes healthy ridges that are minimally resorbed, and well-designed occlusions. However, conventional and optimally made complete dentures are not a panacea for edentulism; numerous patients are prosthetically maladaptive and struggle to adapt to their complete denture wearing and regard the quality of their lives as compromised.
Complete dentures - functional considerations
The foundation for a conventional complete denture is the underlying mucosa, submucosa and alveolar bone. All of these tissues have limited adaptive ability and cannot provide the level of function provided either by teeth and periodontal ligament or by osseointegrated oral implants. The activity of the intra-oral muscles, especially the tongue, leads to denture looseness and can compromise patients’ speech and mastication. Severe ridge resorption is characterized by flat denture bearing areas. In these circumstances dentures slide freely and horizontally. In situations where quality of life cannot be satisfactorily addressed, improving the retention and stability of a denture through use of oral implant anchorage is indicated. For patients who have had difficulties wearing complete dentures, an implant overdenture or fixed implant prosthesis can significantly reduce the impact of time-dependent changes on alveolar bone and functional efficiency.