-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
Crestal/paracrestal Incision
Key points
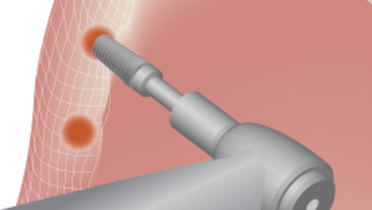
- During the incision the blade must be in contact with the bone to guarantee achieving a full thickness flap
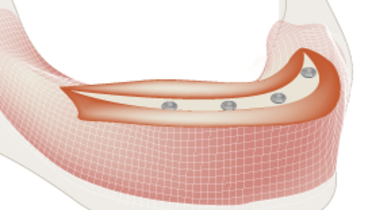
- The keratinized tissue must be separated in order to favor immobile tissue around the implant/abutment
Incision - general considerations
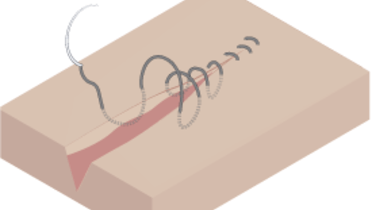
Any intra-oral surgical intervention begins with the incision and finishes with a suture or gluing. Indications for a crestal incision include one-stage surgeries where the implant or abutment is non-submerged and is piercing into the oral cavity after its placement. As a general surgical principle it is not recommended to place the incision on top of a submerged foreign body. However, comparative studies revealed that there was no difference in outcome for endosseous implants with crestal or paracrestal incisions.
Gentle tissue handling will secure the adequate blood supply to the flap, leaving the bone covered with as little blood as possible to keep an adequate visibility of the surgical site.
Maxilla
In the maxilla the incision should be made palatal-crestally. The flap should be full thickness allowing for the visualization of the surgical field. Normally the flap has little flexibility, so a vertical incision in distal areas may be needed. After raising the flap it is necessary to ensure the visualization of the nasal floor, the nasopalatine duct and the buccal and palatal walls.
In a zygomatic implant approach the vertical incisions must be longer and extended towards the zygomatic bone so it can be possible to see the zygomatic arch limits as well the infraorbital foramen.
Mandible
The zone of keratinized gingiva is often reduced in edentuous mandibles. The incision should take into account the position of the mental foramen. When dealing with a severely resorbed mandible where the foramen is lying on top of the crest, a vertical incision in the mid-line can be performed in order to achieve perfect mobility of the flap. After the flap is raised, a perfect view of the field is mandatory, including the visualization of the mental foramen and the buccal and lingual walls.