-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
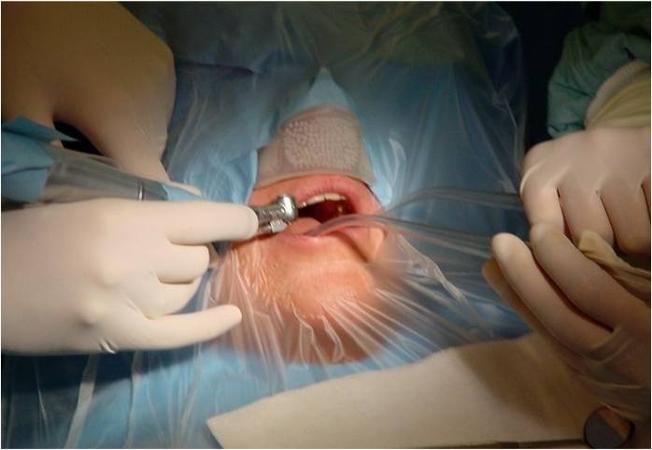
Peri-operative care
Key points
- Peri-operative management of oral and maxillofacial surgery is optimized by familiarity with established protocols and use of surgical safety checklists
- Since implant placement is an elective surgery, contraindications should be thoroughly evaluated and balanced versus the benefit of treatment
Preoperative evaluation
As described in Patient Assessment, a thorough evaluation of patient factors influencing whether to proceed with surgical therapy is relevant.
Depending on the tpe of surgery prescribe pre-operative medication (for example antibiotic coverage), if applicable.
Peri-operative measures immediately prior to surgery
The following list describes important steps to be followed to inform the patient and prepare them properly for imminent surgery:
- Brief information about procedure to ensure that the patient understands and can ask questions about the surgical procedures
- Short acting benzodiazepine can be useful for ambulatory surgery
- If conscious sedation is provided, ensure that an accompanying, responsible adult person will be present with the patient for approx. 3 hours after surgery
- Disinfection of the operative field
- Preferrably cover patient’s nose with a perforated cap to allow for easy breathing and cover face and body with sterile drapes to limit/avoid use of antibiotics
- Use appropriate surgical safety checklist (http://www.for.org/checklists)
Peri-operative care during surgery
The following list describes the important steps to be followed while surgery is being performed:
- Gentle conversations and smooth movements improve patient’s confidence and comfort
- Avoid external pathogens especially from nose by ensuring that the entire team wears masks properly
- The entire surgical team should be trained in asepsis
- If conscious sedation is being provided, the patient's vital signs should be continuously monitored
- If the patient panics, remove surgical fields and interrupt the surgery
- Use appropriate surgical safety checklist (http://www.for.org/checklists)
Peri-operative management immediately after surgery
The following list describes actions and considerations for the patient who has just completed surgery:
- Relaxing seat for ambulatory patients in a quiet environment, which is under supervision, until the premedication effect is over if not accompanied (3 - 4 hours)
- If conscious sedation was provided, ensure that an accompanying, responsible adult person will be present with the patient for at least 3 hours
- Before anesthesia is over, prescribe and/or administer analgesics that do not interfere with coagulation, such as paracetamol or ibupofen
- If significant edema is expected, non-steroidal anti-inflammatory medications are indicated. Opioids should be prescribed/administered only for intractable pain
- Prescribe/administer antibiotic coverage if necessary. If preventive antibiotic therapy has been started before the surgical intervention, this needs to be continued after surgery for 1-4 days and completed according to the antibiotic type used
- Consider to prescribe an antiseptic mouth rinse (e.g. Chlorhexidine)
- Provide brief verbal instructions, including for nutrition. Provide a written summary and 24-hour telephone number to call in an emergency
- Schedule post-operative appointments
- Use appropriate surgical safety checklist (http://www.for.org/checklists)
Clinical topics
Related articles
Additional external resources
Questions
Ask a question
Log in or sign up to continue
You have reached the limit of content accessible without log in or this content requires log in. Log in or sign up now to get unlimited access to all FOR online resources.
No payments necessary - FOR is completely free of charge.