-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
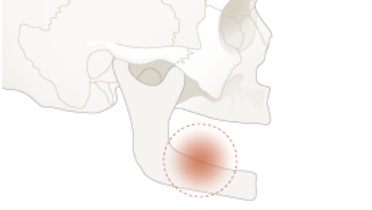
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
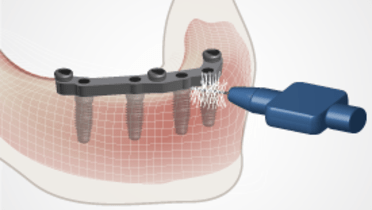
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
Infection - microbiological diagnostics
Key points
- Marginal bone loss can lead to deepened pockets. Superinfection can develop periimplantitis
- Microbiological sensitivity testing, may be clinically relevant when periimplantitis; evidence is present
Microbiota parameters
Presence/number of implants influences aerobe and anaerobe species in saliva and on tongue in edentulism.
Subgingival microbiota in periimplantitis vary according to studies. Less periodontal pathogens than in partial edentulism. Prevotella nigrescens, Fusobacterium nucleatum, P. gingivalis, T. forsythia, Treponema denticola or Aggregatibacter actinomycetemcomitans have been associated with peri-implantitis. Microflora different from periodontitis, with high numbers of peptostreptococci or staphylococci. Typical are enteric rods, staphylococci and yeasts.
Antibiotic medication selection
For periimplantitis the beneficial effects of a systemic antibiotic, as adjunct to mechanincal/surgical treatment remain unproven. Whether the composition of submucosal microbiota is a determining factor for the effectiveness of therapy remains unsubstantiated. Microbial testing can help selecting proper antibiotic by detecting resistant species.
Microbiology tests
Available tests for on an outpatient population:
- phase-contrast microcopy
- culturing
- latex agglutination test
- checkerboard DNA-DNA hybridization
- polymerase chain reaction
Phase-contrast microscopy:
Simple and fast chair-side test which provides proportion of cocci/rods/filaments and motile organisms. Increased % of motile organisms has been associated with aggressivety of periodontitis; this relationship is not established for periimplantitis.
Culturing
Culturing is technique sensitive and time-consuming. Determines sensitivity towards antibiotics. Paper points are inserted in the periimplant pocket and transported in a vial to the laboratory.
Latex-agglutination test
Consists of beads coated with specific antibodies. When contacting target antigens from the sample, à clumping of beads. Simple and rapid.
Checkerboard DNA-DNA hybridization
Optimal test for complex ecosystems. Allows identification of large numbers of species in many samples. ≥104 bacteria allow detection.
Polymerase chain reaction
Involves amplification of DNA sequence by a primer. If amplification occurs, presence of target species proven. ≥ 10 bacteria can be detected. Biofilm may contain enzymes which inhibit reaction.