-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
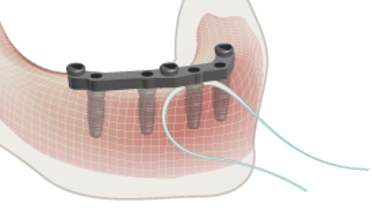
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
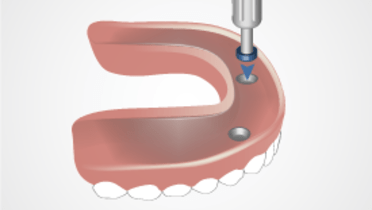
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
Oral hygiene instructions
Key points
- Oral hygiene instructions are one of the most important, yet often overlooked, steps in aftercare
- A properly designed fixed prosthesis is essential to facilitate adequate access for oral hygiene by the patient
- Plaque retention will predispose to mucosal inflammation and pathology as well as unpleasant oral odors
Treatment planning and hygiene considerations
All tissue surfaces, prosthesis surfaces and implant surfaces should be accessible by oral hygiene aids like toothbrushes, interdental brushes and dental floss or dental tape. It is paramount that, during treatment planning, implant location and prosthesis design take place with the final oral hygiene outcome in mind. To this end, all intra-oral prosthesis surfaces should be smooth and highly polished to counteract plaque retention.
Oral hygiene instructions - patient
Every visit should have oral hygiene instruction incorporated, and the instruction should potentially need review. This is especially important for fixed prosthesis. Oral hygiene instruction should be pursued until the patient can demonstrate independent competence accessing all pertinent intra-oral areas using the appropriate oral hygiene aid. Although most patients can clean well with a regular toothbrush and dental floss, special brush forms are available to clean around implant-supported restorations. There seems no difference in outcome between powered and manual toothbrushes.
Removable prosthesis
Removable prostheses should be removed every night by the patient and kept in a humid atmosphere or soaked in water or denture cleanser. Abutments and prosthetic superstructures retaining removable prostheses should be brushed scrupulously to be kept plaque-free and ensure optimal mucosal health. Inflamed mucosal tissues may result from inadequate plaque removal.
Caretakers/dependent patients
To also make the caretakers familiar with the recommended hygiene measures, the dentist/dental hygienist should consider to associate caretakers to the instructions for aftercare for (elderly) dependent patients.