-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
Implant overdenture maintenance
Key points
- Use recall visit to check overdenture and restorative components for adjustment needs
- Both attachment matrix activation and replacement are commonly encountered
- A symptomatic growth of hyperplasic soft tissue around implants and particularly underneath bars is commonly seen and usually rectified by a program of vigorous massage
Implant Overdenture Maintenance
The objective of systematic periodic recalls for patients wearing overdentures are three-fold:
- to check the overdenture for minor denture adjustments, retention, stability, occlusal adjustments and maintenance of employed attachment system
- to monitor peri-implant marginal bone and peri-implant soft tissues
- to control and adjust the level of oral hygiene
Published long-term reports indicate that both matrix activation and replacement are commonly encountered. Moreover, replacement of denture teeth, rebasing, relining or remaking of the implant overdenture together with wear and tear of the ball abutments or connecting bars (patrices) occur more frequently after a few years. The type of attachment system used also influences the frequency of prosthodontic maintenance events required: ball attachments and locators need more frequent maintenance.
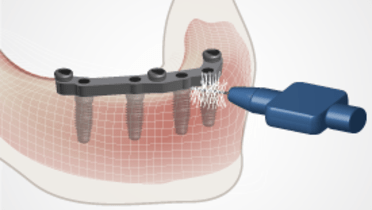
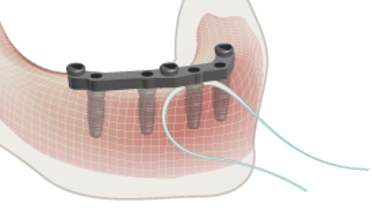
Cleaning and hygiene
The cleaning of implants and overdentures is clearly easier when compared to fixed full-arch prostheses. The majority of patients with overdentures who are in special need of oral health care are frequently elderly. They often have to cope with impaired manual skills and reduced visual capacity. They are also likely to have difficulties in following cleaning instructions and have to rely on their care providers for professional assistance. They have to be taught individual hygienic procedures that best correspond to their abilities.
The wearing of overdentures certainly enhances plaque accumulation and candida/fungal infections. Therefore, the patients should always be instructed NOT to wear their prosthesis at night.
Hyperplasic soft tissue
A symptomatic growth of hyperplasic soft tissue around implants and particularly underneath bars is commonly seen. Renewed oral hygiene instructions and/or the use of antifungal paste, can rapidly get rid of this phenomenon. Sometimes, surgical (laser-therapy) is indicated to decrease soft tissue overgrowth.
Caretakers/dependent patients
To also make the caretakers familiar with the recommended hygiene measures, the dentist/dental hygienist should consider to associate caretakers to the instructions for aftercare for (elderly) dependent patients.