-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
Choice of implant
Key points
- Most modern implants rely on a combination of commercially pure or alloyed titanium, threaded designs and moderately rough surfaces
- Implant systems are available in various dimensions to address individual anatomical and implant site conditions
- Review of the scientific basis and clinical track record of the various available implant systems and their implant design and surface features can assist in the selection of an adequate implant type
Implant design
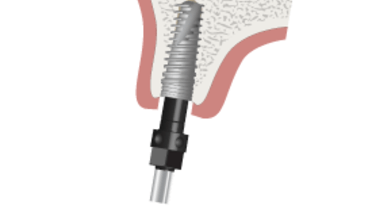
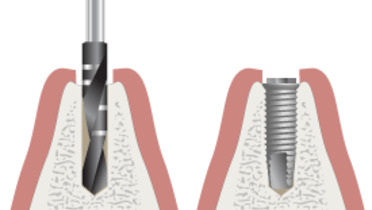
The majority of commercially available implants are variations of Brånemark’s original design of a screw which he coined as 'fixtures'. This has been the starting point for numerous current market variations that incorporate convergent themes of implant material, size, macroscopic and microscopic features. They all rely on a combination of commercially pure titanium (Brånemark’s original material choice), threaded designs and moderately rough surfaces. They are available in a diversity of dimensions that lend themselves to the different treatment plans that seek to exploit diverse, naturally occurring or optimally modified, selected host sites for implant placement (Tapered implant placement, parallel implant placement)
Scientific considerations
Oral endosseous implants are characterized by different degrees of scientific pedigree. They demonstrate a range of subtle and sometimes even profound design shifts from Brånemark’s original prototype, all claiming maximization and optimization of the induced interfacial healing response of osseointegration. There are also limited long-term clinical outcome results about the use of titanium alloys, HA-coated and porous-coated implants. Furthermore, bioactive and nanosurfaces remain topics of research interest. They are undocumented as far as long term clinical efficacy and effectiveness outcomes are concerned.
Osseointegration
Osseointegration results from the convergence of three key variables. The first variable is the inherent healing potential of the patient. Several clinically relevant factors such as smoking, some medications and some systemic diseases have been identified (see Risk assessment).
The second variable is the combined surgical and prosthodontic judgment and dexterity of the clinician. Last, and by no means least, is the choice of implant. It is essential to check the available scientific documentation on clinical outcome. Extrapolation of data from an implant system which looks similar is unacceptable.