-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
Soft tissue management
Key points
- The need for keratinized/immobile soft tissue surrounding permucosal implants remains a matter of debate
- Maintenance of inflammation-free peri-implant soft tissue may be easier when immobile
Aims of peri-implant soft tissue management
The aims of peri-implant soft tissue management in the edentulous mandible are the eventual reconstruction of attached gingiva or immobilizing the soft tissue at the implant-soft tissue interface. Vestibuloplasty means deepening of the vestibule.

Techniques and grafts for soft tissue management in the edentulous mandible
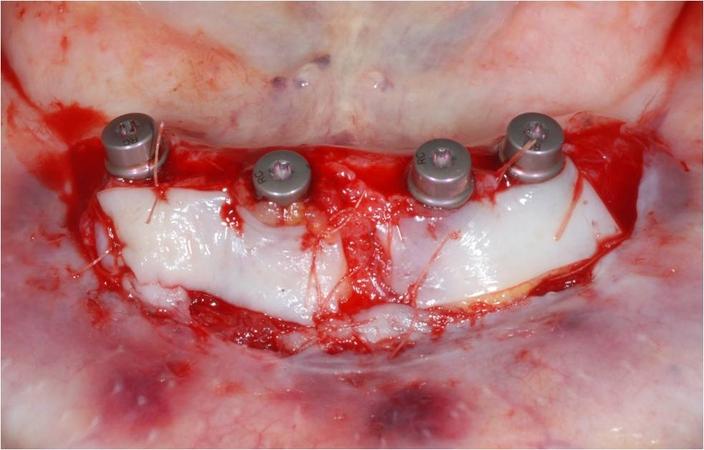
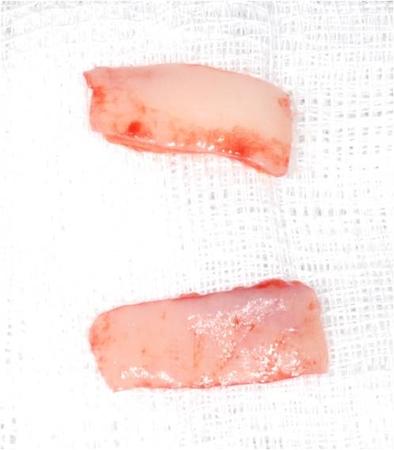
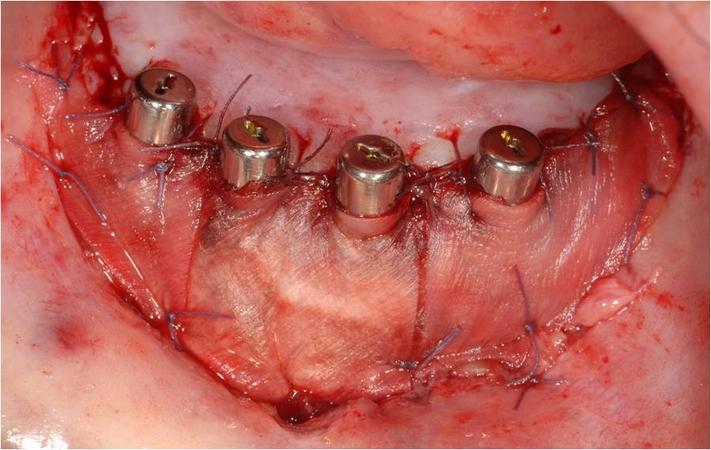
Depending on the soft tissue deficiency and its localization, different techniques and tissues are used to generate a sufficient band of keratinized mucosa around permucosal implants. Traditionally free soft tissue grafts are used for augmentation. Free gingival grafts from the palate and the retromolar pad are the current standard augmenting technique for small peri-implant areas when keratinized gingiva is needed (Fig 2). The use of free gingival grafts is limited (graft dimension: 10 x 30 mm), due to availability and morbidity. Recently, animal-derived graft materials (such as porcine collagen matrices) have been introduced into peri-implant soft tissue reconstruction (Fig. 3).
Deepening of the vestibule can be indicated to meet prosthetic demands such a retention of complete dentures or providing space for flanges of an overdenture. Deepening of the vestibule has a tendency to quickly diminish after few years. The combination of vestibular deepening with implant-based therapy seems the best option.
Success and limitations of peri-implant soft tissue management
The success depends on the shrinkage of the reconstructed soft tissue. In studies, animal derived matrices showed similar clinical outcome as free gingival grafts. There is insufficient information to recommend which is the ideal graft and and which is the best technique to increase the width and thickness of keratinized/ attached gingiva.