-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
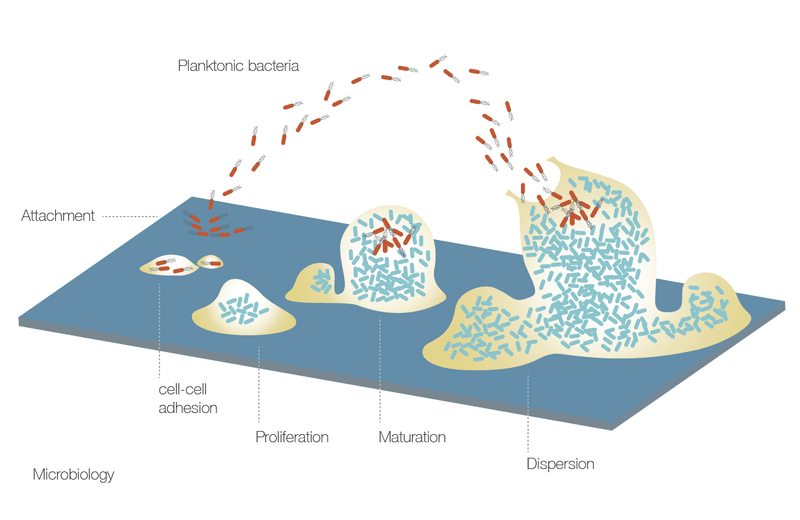
Microbiology
Key points
- Microbial testing is not necessary before implant treatment
- Decreasing microbial load in saliva of edentulous patients is easily achievable by tongue scraping and oral rinses with antiseptics
- Only when implants are in place and superinfection occurs can microbiological sensitivity testing become clinically relevant
Oral microflora
Epithelial desquamation in the oropharynx limits bacterial accumulation, except on the tongue dorsum and in the tonsillar crypts. Loss of teeth dramatically reduces the load of periodontal pathogens except for Aggregatibacter actinomycetemcomitans and to a lesser extent for Porphyromonas gingivalis. In the absence of subgingival pockets, they survive on the dorsum of the tongue, in the tonsillary crypts or other parts of the oropharynx.
Microbial testing considerations
With reference to implant therapy, there is no convincing evidence to demonstrate the impact of salivary microbial load and composition in patients with a history of periodontitis on implant treatment outcomes. Therefore, the relevance of microbial testing prior to implant treatment is unproven. Preoperative asepsia in edentulism can be easily achieved by daily tongue cleaning and the use of antiseptic rinses like chlorhexidine digluconate 0.1–0.2 vol%, just prior to implant-surgery. The administration of pre-operative antibioticis, in not-compromised patients, has therefore also no significant evidence.