-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
Hyposalivation and Xerostomia
Key points
- Saliva plays a significant role in the preservation and maintenance of oral health and function, as well as in patients’ ability to tolerate removable dentures
- Hyposalivation can be caused by age-related decline in salivary gland function, dehydration, therapeutic medication, head and neck radiotherapy, some autoimmune disorders, metabolic disorders (diabetes) etc.
- Xerostomia diagnosis is based upon patient history, especially complaints of nocturnal dryness, and oral examination
- Typical symptoms comprise dry cracked lips, angular cheilitis, dry tongue, oral candidiasis, swallowing difficulties and reduced denture wearing comfort
Saliva - function
Saliva plays a significant role in the preservation and maintenance of oral health and function. It supports digestion by preparing food for mastication and swallowing, contributes to taste perception, facilitates speech communication and provides oral tissues protection from dessication, microbial penetration, or ulceration. Saliva can also stimulate soft tissue repair by reducing clotting time and accelerating wound contraction. The quality (viscosity) and quantity (flow rate) of saliva are crucial factors in patients’ ability to tolerate removable dentures since thick, ropey saliva tends to dislodge them; while thin or low salivary flow provides an insufficient film for their retention and mucosal lubrication.
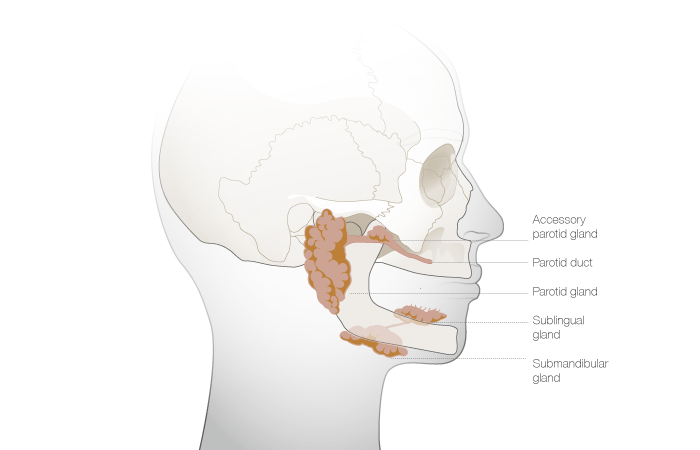
Hyposalivation and xerostomia etiology
Hyposalivation, and the accompanying state of patient perception of dry mouth (Xerostomia), are a frequent complaint in the eldery patient. This is primarily because of dehydration, therapeutic medication (especially parasympathetic drugs), head and neck radiotherapy, autoimmune disorders (e.g. Sjögren’s syndrome), rheumatoid arthritis, diabetes or age-related decline in salivary gland function.
Xerostomia symptoms
It may leave patients susceptible to dry cracked lips, angular cheilitis, dry tongue, oral candidiasis and swallowing difficulties. Dry mouth compromises denture wearing comfort because of associated chewing and speaking problems as well as soreness and irritation of denture-bearing areas.
Diagnostic considerations
Its diagnosis is based upon patient history, especially complaints of nocturnal dryness. There is no single test (yet) that can confirm diagnosis. Upon oral examination a tongue depressor may actually stick to the buccal mucosa. The most common and most severe dry mouth disorder is Sjögren’s Syndrome (SS) - a chronic inflammatory autoimmune disorder that can appear at any age. It takes anywhere from 5-9 years for SS to be diagnosed definitively and clinicians should be alert to patients with histories of reduced salivary flow and investigate further via appropriate medical consultations.
Implant treatment
Some literature justifies prescription of implant supported prostheses for edentulous patients with hyposalivation/xerostomia. This is on the presumption that stable and optimal prosthodontic occlusions may contribute synergistically to salivary gland stimulation for lubricated bolus formation and oral mucosal protection. Moreover several case reports indicate considerable improvements in comfort and function for this group of patients.