-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
Prosthodontic Options - overview
Key points
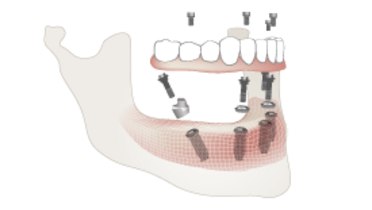
- Implant-based restorations offer patients improved chewing function, facial/dental esthetics, increased quality of life and self-esteem
- A fixed, implant-supported prosthesis is most likely to feel like the patient's own teeth
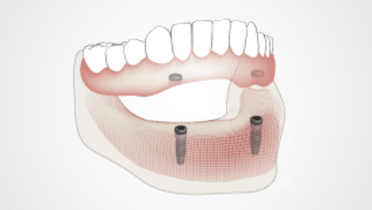
- Removable implant overdentures offer a high value treatment option with significantly enhanced retention and function compared to conventional removable dentures
Fixed implant prostheses
Fixed implant prostheses are associated with the best oral health and quality of life, as chewing performance and patient comfort are usually better than with a removable prosthesis. The use of all-ceramic, metal-ceramic or metal-resin prostheses offers a variety of treatment options to address specific patient needs.
Implant overdentures
Complete denture wearers experiencing a poor quality of life may have oral implants placed to support or retain an overdenture. Since these denture wearers suffer from poor denture retention and denture instability that manifests during mastication and speech, the use of oral implants addresses the retention and stability goals. Implant overdentures may use attachments that are directly placed on the implants or may use a bar superstructure on which attachments are placed. The attachments are usually resilient in nature allowing tissue-ward movement of the prosthesis during functional loading. These prostheses are removable and the patient can insert and remove them for cleaning and oral hygiene measures.
Conventional complete dentures
Conventional dentures rest exclusively on mucosa and all chewing forces are transferred to this vulnerable tissue. Mandibular dentures, because of the activity of the tongue, have a poorer prognosis than maxillary dentures which also have a greater surface area to distribute functional forces. Conventional dentures can work well for patients who are adaptable and have a history of successful conventional complete denture wearing. Also, well-made dentures may be a solution in regions or situations, when implant-based treatment is not available. For patients who have struggled to enjoy a good quality of life with conventional dentures, the advent of oral implant therapy has significantly improved chewing function, esthetics, patient self-esteem and social confidence.