-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
Age
Key points
- In elderly patients consider reduced bone metabolism and extended healing and integration times. Interventions should be minimally invasive
- In elderly patients consider prosthetic superstructures in a straight-forward design to allow for easy hygiene measures. Removable prostheses are preferred after years of edentulism
- In the rare case of juvenile patient anodontia or juvenile edentulism, an implant-supported fixed tooth replacement may be considered at an early age
Agenesis & edentulism in juveniles
Edentulism as a consequence of (sub)total agenesis of deciduous and/or permanent teeth in children and adolescents is extremely rare. It is commonly a component of a generalized underlying condition such as ectodermal dysplasia. There are different subtypes such as hypohidrotic ectodermal dysplasia, often associated with mental retardation. The external appearance and shape of the juvenile edentulous mandible will depend on the presence of deciduous teeth.
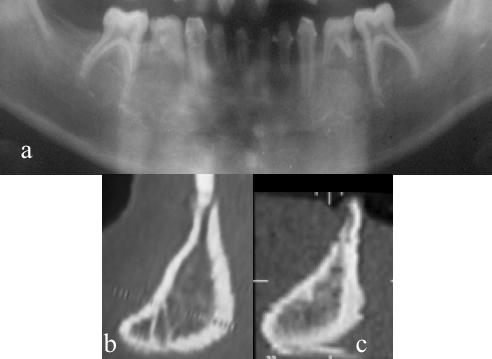
In patients with development of deciduous teeth but missing permanent tooth buds, a high, but extremely narrow alveolar process will be found. After the loss of the deciduous teeth, the alveolar process will show a shape being pointed in occlusal direction (Fig 1).
However, in patients with simultaneous agenesis of deciduous teeth, the outer appearance and shape of the mandible is characterized by a virtually complete lack of the alveolar process associated with a reduction of the local growth potential.
Edentulism in advanced age
Development of edentulim during adulthood will lead to alveolar ridge resorption over time. In elderly patients changes in the external appearance and shape of the jaws will also be accompanied by osseous metabolic changes. Cellular activity of the bone as well as neoangiogenesis is clearly reduced with advanced age. Bone healing is consequently substantially prolonged in elderly patients. As a result, the number of bone-implant surface contacts tends to decrease with increasing age. However, even advanced age has not been shown to be a risk factor for implant failure.
Consequences for the treatment of juvenile patients
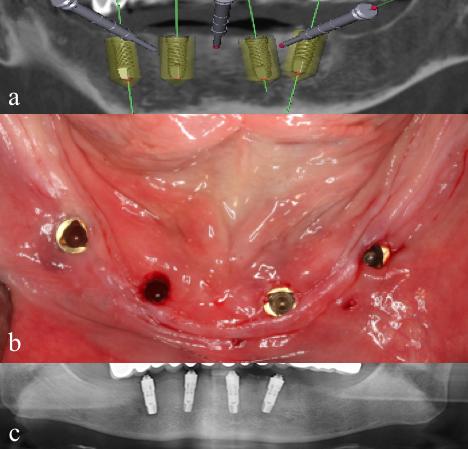
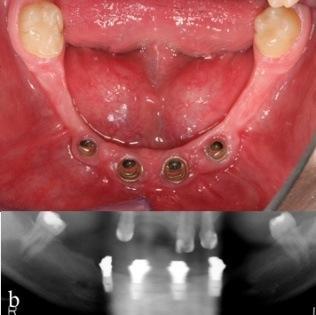
Early prosthetic rehabilitation of such patients influences favorably the direction of growth of both the maxilla and the mandible. Such treatments should only be performed in highly qualified centers. In patients with extensive dental aplasia, implants can already be placed at an early adolescent age considering the rather limited growth in some areas (Fig 2). Change of abutment lengths and prosthetic superstructures can cope with some growth.
Consequences for the treatment of patients with advanced age
If possible, all procedures and interventions should be minimally invasive and implant healing and integration times are to be extended. For bone augmentation procedures prolonged healing times should definitely be observed.
Prosthetic superstructure should allow for convenient oral hygiene in order to compensate for any age-related loss of manual dexterity or general frailty. If the patient has been edentulous for some time and is used to removable dentures, he/she will often prefer a removable overdenture over a fixed reconstruction.
Upon appropriate observation of these guidelines the prognosis for the implants will be similar to the prognosis for “standard patients” (Fig 3).