-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
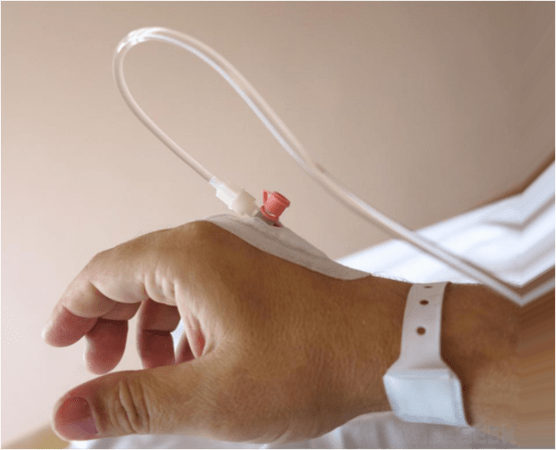
Anesthesia
Key points
- Choice of anesthesia should be defined by what is best for the patient
- Staff members must be properly trained in resuscitation procedures and available equipment
- Intravenous sedation, depending on the drug, may lead to conscious sedation or general anesthesia
- General anesthesia: Loss of consciousness, patients not arousable, even by painful stimulation
- For elected procedures, general anesthesia should be considered with care
- During conscious sedation, verbal contact with patient is maintained
General Considerations
The choice of anesthesia depends on many variables including the complexity of treatment, duration of treatment, need for patient awareness and the response during treatment, only to name a few. In general, the clinician and patient should discuss the risks and benefits of possible anesthesia and sedation types and select the type that provides the minimum adequate amount of anesthesia and sedation needed to complete the treatment procedure. Guidelines regarding the patient's medical condition regarding anesthesia should be followed carefully.
The two main types of anesthesia/sedation include infiltration with local anesthetics and regional anesthesia with local anesthetics. Either type of anesthesia can be combined with conscious sedation. In cases of complex surgery, general anesthesia may be considered and the patient should be referred to a highly trained specialist who is experienced in the use of general anesthesia.
Infiltration with local anesthetic
- Mostly lidocaine, articaine or mepivacaine with or without a vasoconstrictor in a carpule that is deliverd though syringe injection
- Bevel of needle should be parallel with periosteum
- Slow injection of anesthetic warmed to body temperature
- Topical anesthesia should be used prior to injection
- Duration of anesthesia varies with patient metabolism and anxiety
Regional anesthesia with local anesthetic
- Inferior alveolar block anesthesia for pain control in distal mandibular areas
- In frontal areas of non-resorbed jaws where there is less corticalized bone local infiltration is often sufficient
- A more technique-sensitive process than local inflitration
- Aspiration is mandatory since 5% of aspirations are positive and need reorientation of needle and reaspiration or else new injection with reaspiration
- Facial nerve may be temporarily paralyzed
Conscious sedation
- Usually combined with local anesthesia
- The patient remains conscious and can respond appropriately to verbal commands
- Nitrous oxide and oxygen administered through the nose. Nitrous oxide has sedative and analgesic effects
- Intravenous (IV) delivery of benzodiazepines is a safe and widely-used method for obtaining conscious sedation
- There are contraindications to conscious sedation such as pregnancy, allergy and alcohol intoxication. Therefore, a thorough medical history is important
- Resuscitation equipment, a positive-pressure oxygen delivery system and an intubation tube should always be available during conscious sedation
- National regulations regarding administration of conscious sedation should be followed
General anesthesia
- In general anesthesia there is a complete loss of consciousness, amnesia, analgesia, relaxation of skeletal muscles and loss of control of the autonomic nervous system
- Therefore, general anesthesia should only be provided in hospitals or equipped medical centers and where essential postoperative facilities under medical surveillance are available
- The use of preoperative clonidine or benzodiazepines reduces the dose of anesthetics needed
- Physiologic monitoring and airway management are mandatory
- Duration of anesthesia is normally not an issue