-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
Occlusion check
Key points
- Malocclusion is the most common cause of prosthetic failure
- Careful attention to establishing bilateral and stable occlusion is imperative
- Harmonious occlusion significantly enhances the function and longevity of dental prostheses
Evaluation of occlusion
In the rush to meet patient demands for functional rehabilitation, the importance of occlusion is often overlooked. A check of the occlusion should be performed at every visit from insertion onwards because many problems with fixed dental prostheses can be traced back to malocclusion. They can cause pain, restoration failure, compromise phonetics and masticatory function. Implants do not have the shock-absorbing capacity of a periodontal ligament. Implants do not provide the same occlusal awareness to patients as their natural dentition.
Occlusion concepts and principles
The ideal occlusion remains a matter of endless debate. Depending on the geographic area either a balanced occlusion or a canine guidance for example can prevail. All epidemiological studies demonstrate the widespread occurrence of of occlusal interferences and that there are more people with non-ideal functional occlusal relationships than people with symptoms of functional disorders. Nevertheless when a fixed or removable prosthesis is planned on implants to rehabilitate an edentulous patient, some occlusal principles should be respected.
Several occlusal concepts, such as balanced, group-function, and mutually protected occlusion have been extrapolated to implant-supported prostheses. There is no sufficient evidence to suggest that a specific occlusal scheme is superior for implant-supported prostheses. There is a general tendency for flat occlusal fossae and grooves for wide freedom in centric. Bilateral balanced occlusion has been proposed for cross-arch fixed prostheses when opposing a complete denture, while group-function occlusion has been widely adopted for opposing natural dentition.
When a cantilever is utilized in a cross-arch fixed prosthesis, infraocclusion of the cantilver unit may avoid material fatigue.
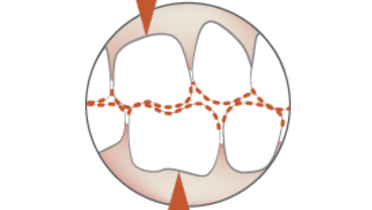
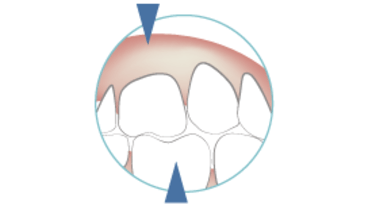
Considerations for underlying mucosa
Occlusion is extremely important with removable dental prostheses as the underlying mucosa was not evolutionarily selected to directly withstand occlusal forces generated during chewing. This is especially true for movable and non-keratinized mucosa. There is no doubt that creation of a bilateral and stable occlusion enhances the probability of patient comfort and prosthesis success, and assists in preventing development of pressure sores.