-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
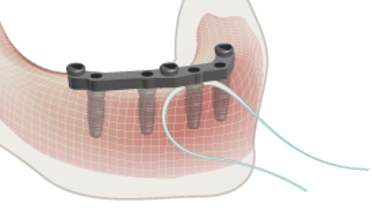
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
Patient Demand
Key points
- Examine why the patient is seeking treatment and assess patient motivation for treatment
- Examine whether patient expectations match patient demands
- Discuss assessment results for treatment options and treatment planning
- Be cautious to not overpromise treatment possibilities and results
Esthetics, function, comfort, quality of life
In order to provide adequate treatment and meet patient satisfaction, it is crucial to evaluate patient expectations. These expectations normally fall into one or more of four categories: function, comfort, esthetics and quality of life. The patient interview should elucidate those factors that are of the greatest importance to patient satisfaction. A typical patient interview would include the following:
- Why the patient is seeking treatment
- The patient's chief complaint(s)
- If there are quality of life issues and challenges
- Is the patient currently in pain or discomfort?
- How important is the esthetic outcome and what are esthetic expectations?
- Is the patient looking for improvement in speech or mastication?
- Does the patient feel a lack of confidence and/or self-esteem in social situations?
Considerations and influence on treatment planning
Beyond a thorough discussion about expectations, an assessment should be made with regard to some additional treatment planning influences.
- Is the patient interested in a complete rehabilitation or is he/she focused on the anterior (esthetics) or posterior (function) zone?
- Is the patient amenable to surgical procedures or is he/she seeking only non-surgical alternatives?
- Is the patient interested in either only a fixed or only a removable prostheses?
- What is the patient's professional background and what are his/her social obligations?
Above-mentioned themes will influence and guide treatment planning options, e.g. respective number of implants, selection of retention elements (e.g. ball abutments only, bar, fixed or removable, cement-or screw-retained constructions), full ceramic options or PFM / alloys, and requirements for the provisional solution. The patient's professional background and requirements may affect esthetic and functional requirements in general, but also during the provisionalization phase.
Patient expectation management and guidance
Understanding and successfully managing patient expectations is the most important predictor of patient satisfaction. Therefore, the clinician should very carefully evaluate how a patient expresses his/her demands during the first discussion and how patient adapts their expectations after hearing what can and cannot be achieved by different treatment options. One should not overpromise treatment possiblities. To that end, during the discussion of treatment options and the key factors associated with each option, the following concepts should be presented to the patient:
- What is possible to achieve and what is not
- Prognostic factors including age, motivation, dexterity and ability to present for regular recall appointments
- Treatment times & timelines
- Costs and eventual reimbursements
- Importance of compliance / patient time and efforts
- Behavioral adaptation and restrictions during treatment time (e.g. smoking, certain food/masticatory habits, social life, temporary discomfort etc.)
- Morbidity
- Risks
- Forensic aspects

The occurrence and response to the treatment options discussion must be documented in the patient record including a review of the different treatment options presented.