-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
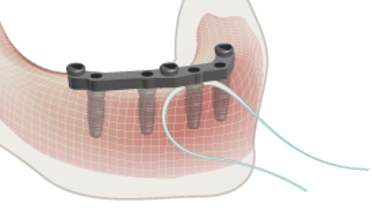
2.2
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
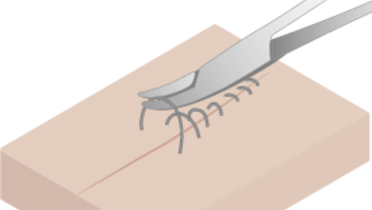
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
Recall visits - overview
Key points
- Plan a regular recall control appointment, preferably at least every 6 months
- In situations of compromised patient health and/or oral hygiene, increase recall frequency and hygiene measures
- Evaluate whether patient expectations have been met and quality of life improved
- Examine the condition of soft and hard tissue and prosthetic components and render necessary maintenance
Regular recall controls - important for long-term treatment success
To achieve good long term results, regular recall control appointments should be scheduled. Ideally, recall appointments take place at least every 6 months for a systemic review of the general health, medication and oral condition of the patient. Depending on motivation and oral hygiene level, the clinician may consider an increased frequency of recall visits.
Check list for important recall visit activities
- Are patient expectations met and quality of life improved?
- Evaluate general health of the patient, patient compliance and oral hygiene
- Professional prophylaxis by dentist, hygienist, or assistant.
- Check for loose restorations (de-cementation, broken or loose screws) and wear of prosthesis
- Check for chipping and fracture of prosthesis elements
- Check function of retention elements of implant overdentures
- Check occlusion and function
- Examine for signs of inflammation, infection, swelling, exudate, pus, pain, bleeding, plaque, peri-implantitis and/or mucositis
- Obtain radiographs at appropriate time frames based upon recall or presence of concerning signs/symptoms
- Review medications and update changes to medication history accordingly
- Schedule next recall visit
Clinical topics
Related articles
Questions
Ask a questionInt J Dent Hyg. 2011 Aug;9(3):216-22.
Log in or sign up to continue
You have reached the limit of content accessible without log in or this content requires log in. Log in or sign up now to get unlimited access to all FOR online resources.
No payments necessary - FOR is completely free of charge.


shortage in reference
Int J Dent Hyg. 2011 Aug;9(3):216-22.
Int J Dent Hyg. 2011 Aug;9(3):216-22.