-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
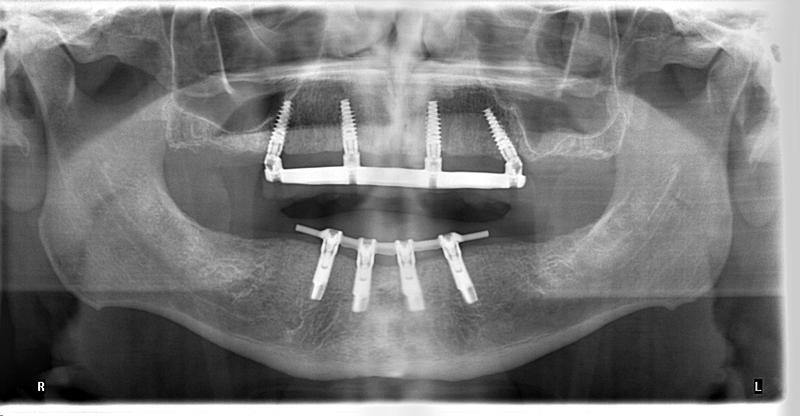
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
Number of implants maxilla and mandible
Key points
- Since surgery to deal with edentulism belongs to elective surgery, one should consider the risk-benefit ratio and opt for less invasive surgery when patient needs and wishes can thus be met
- When opting, in agreement with the patient, for either fixed or removable prostheses besides financial costs, the “cost” of discomfort, risk of complications, unavailability to normal activities, treatment duration … should all be considered.
- Removable (bar-retained) prostheses can sometimes be easier to maintain plaque-free by elderly patients.
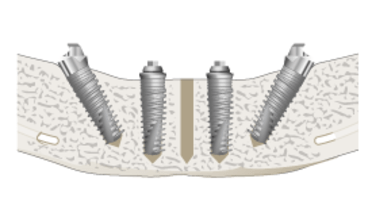
- In the mandible an overdenture on two implants in the symphysis, connected or not by a bar, is the standard of care for patients who have been edentulous for some time.
- Excellent survival rates (> 99 %) are reported in the maxilla with ≥ 4 implants supplied with a bar anchorage for an overdenture or to carry a fixed prosthesis
Fixed Prostheses
Number of implants and implant design evolution
The tradition to insert 6 implants, and eventually more, in an arch-wide pattern dates back to the early days of osseointegration when implants with a machined surface were used and risk for early non-integration was an issue. Thus, if one implant was lost, no extra insertion during revision surgery was needed. The prosthesis could remain functional. With the presently available implants with slightly rough surfaces achieving very high survival rates, the placement of supplementary implants, just to avoid revision surgery should a failure occur, cannot be justified. There may be exceptions for medical conditions which render any surgery risky, or when the jaw bone is seriously compromised.
Traditional and anecdotal approaches
The anecdotal/traditional reports, inserting one implant for each tooth, to rehabilitate an edentulous maxilla, are not based on any biomechanical or physiological arguments. Inserting as many implants as possible interferes with soft tissue healing and oral hygiene.
Current, minimally invasive approach and considerations
For cross-arch fixed prostheses, which cannot achieve a perfect passive fit, because CAD/CAM technologies were not used, more than 4 implants are needed to deal with segmentations of the framework. When only a limited jaw bone volume is available, especially if it avoids augmentation procedures such as sinus inlays or mandibular onlays, the use of 4 implants only, eventually with the distal ones tilted, offers a well-documented excellent treatment outcome. Tilting of the two distal ones backwards achieves a better anterior-posterior spread which is biomechanically rewarding. Tilted implants demonstrate the same marginal bone change over time as the axial ones.
When special esthetic or phonetic endeavors have to be met, or when medical conditions render any further surgical intervention risky, it may lead to using 5 implants and even more to support a fixed prosthesis in the maxilla.
Overdentures
In the lower jaw, two implants placed parallel with the hinge axis of the mandible allows to have an overdenture which can rotate to a certain extent. The distal parts of the denture are thus mucosally supported. Excellent long-term ( > 10 years ) survival rates ( ≥ 95 %) have been reported. Especially in young patients where such treatment will be maintained for decades it may be wise to opt for 4 implants interconnected by a bar, so that the distal parts of the mandible do not resorb due to the denture loading.
Elderly patients, who have been denture wearers for years, may express a preference for overdentures to a fixed prosthesis.
Even one symphyseal implant seems to suffice to retain an overdenture.
In the extremely resorbed mandible 4 short implants could be placed. When the bone height is <6 mm, a bone augmentation procedure is advised
In the maxilla overdentures should be retained by ≥ 4 implants. With such retention system, medium term survival rates of ≥ 99 % are common. There is no difference in outcome between substructures on 4 or on 6 implants in the maxilla.