-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
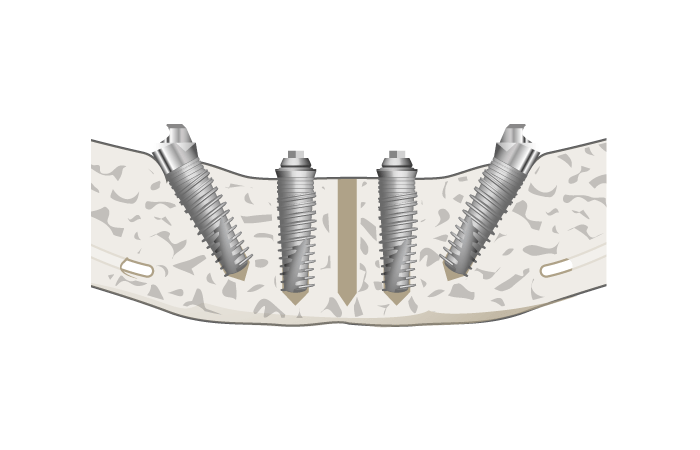
Placement of implants - Angulation
Key points
- Treatment with properly angulated implants compensates for the pseudo-progeny in the edentulous mandible
- Properly angulated implants overcome clinical situations with minimal posterior bone support in the edentulous lower jaw
- Use of angulated implants reduces the need for ridge augmentation
- Use of angulated implants allows for a fixed prosthodontic rehabilitation in the edentulous maxilla and mandible
Aims of angulated implant therapy
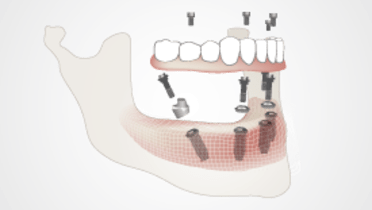
The primary goal of angulated implant placement concepts is the implant-based prosthodontic rehabilitation of the edentulous maxilla and mandible and avoiding grafting procedures and thereby offering a more simple and less invasive treatment alternative for a fixed full-arch rehabilitation. The implant-based prosthodontic rehabilitation of the edentulous patient is optimized due to the reduced cantilever-length.
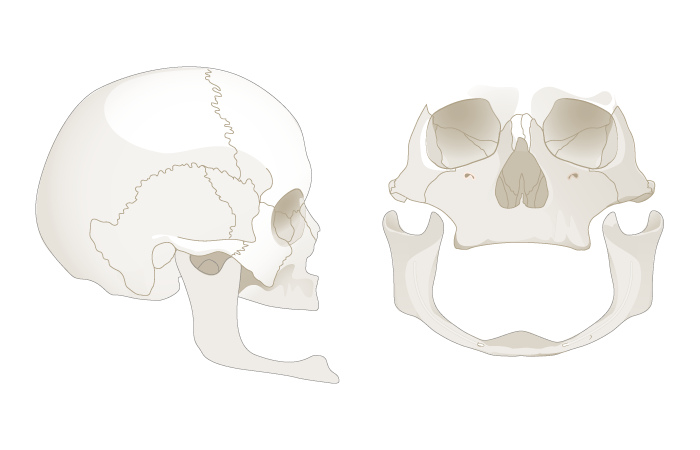
Treatment concept
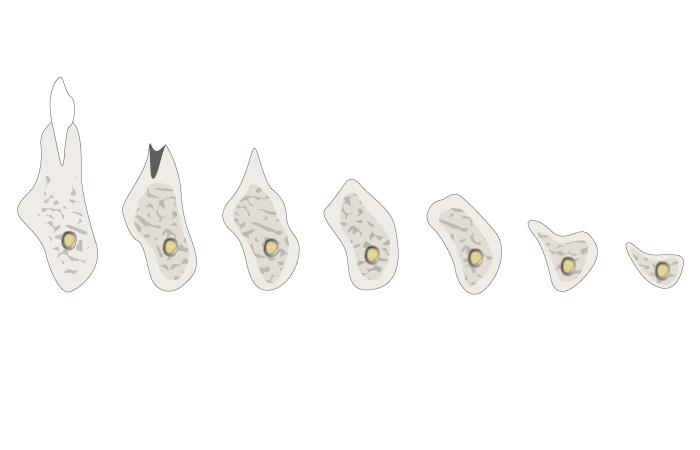
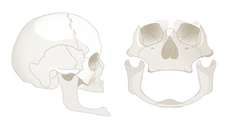
Loss of vertical dimension (Fig 3) in the edentulous patient leads to loss of sagittal projection of the maxilla and mandible (Fig 2). The resulting pseudo-progeny can be compensated through the backward inclination (anterior-posterior dimension) of angulated implants.
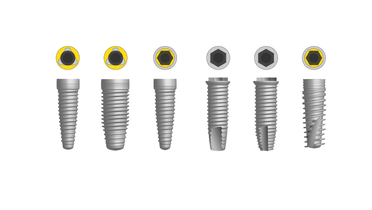
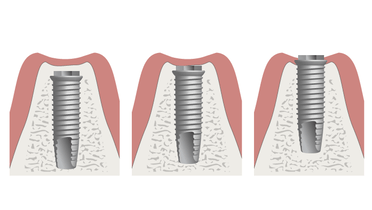
In the posterior maxilla, atrophy leads to insufficient bone height between the alveolar crest and the floor of the maxillary sinus. The need for sinus grafting can be avoided through placement of angulated implants. In the posterior edentulous mandible atrophy leads to a reduced vertical bone height which can make implant insertion difficult. The need of pre-implant orthognatic surgery, augmentation procedures or nerve displacement can be circumvented by placing distally angulated implants in the edentulous mandible. Respecting the anatomy of the mental nerve and the atrophic posterior regions of the edentulous mandible (Fig 2), the distal angulation of intraforaminal implants allows for a short cantilever length and large inter-implant distance (Fig 1). Using angulated orientation for implants allows for the use of longer implants.
Pre-surgical preparations for placement of angulated implants
Angulated implant insertion in the edentulous patient requires pre-surgical planning. Pre-surgical impressions allow for the fabrication of a conventional splint which will define the drilling angulation. In order to obtain an increased precision of the implant insertion a CT or cone-beam computed tomography (CBCT) can be performed. Planning software is used to simulate implant number, length and angulation. Subsequently a surgical stereolithographic template for guided implant insertion is designed according to the 3D treatment plan. Insertion of implants can be performed by guided surgery according to the position and angulation of implants, given by the template.