-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
Placement of implants - Height
Key points
- Implants can be placed supra-, equi- and subcrestally
- After implant placement bone remodeling processes take place and a periimplant soft and hard tissue interface is established
- Implant insertion depth is dependent on implant collar design and implant surface treatment
Aims after implant placement
The overall aim after implant placement concerning the periimplant bone height is to minimize marginal bone loss. However, several bone remodelling processes that occur after implant placement lead to periimplant bone loss and the establishment of a soft tissue interface. It has been hypothesized that implant neck designs and implant insertion depths, in particular the positioning of the implant shoulder in relation to the alveolar bone crest may impact on crestal bone resorption observed around endosseous implants.
Implant depth positioning
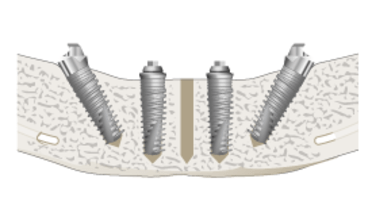
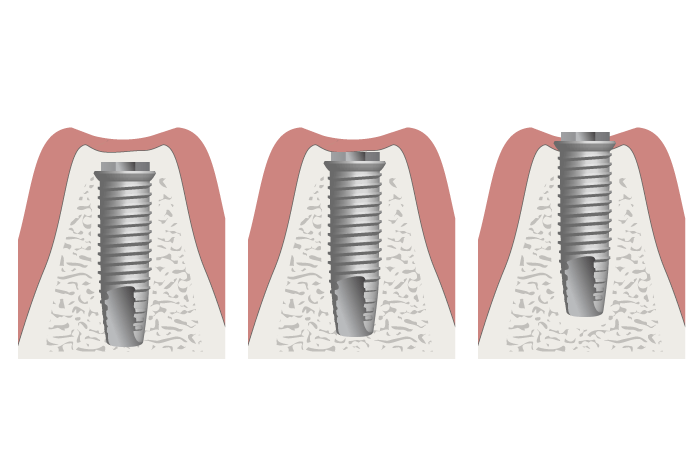
With regards to implant height, oral endosseous implants can generally be placed supra-, equi-, and subcrestally (Fig 1).
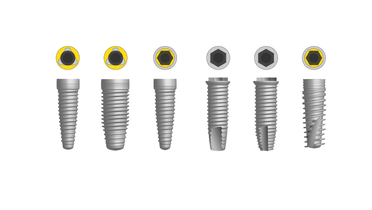
Since there are differences in implant collar/neck designs and surface treatments there are system-dependent differences of implant insertion depths. Briefly, one should distinguish between implants with a rough surface implant neck and implants with a smooth surface machined implant neck.
In general, the rough surface of the implant will be surrounded by bone. This means a subcrestal or equicrestal insertion of implants with a structured implant surface up to the implant shoulder and a supracrestal insertion of implants with a machined implant neck. No matter which implant system is chosen, the exposure of the implant surface in the oral cavity, especially its rough component should be avoided in order to prevent from unwanted plaque accumulation and periimplant inflammation.
Subcrestal positioning of implants has been proposed to decrease the above-mentioned risks. Even though the subcrestal placement might reduce the distance from the implant shoulder to the first bone-to-implant contact and promote a soft tissue interface in a most coronal position, it might not have any effect on minimizing crestal bone loss.
Recommendations
Concerning implant insertion depth it is recommended to follow system-specific recommendations. One should always ensure that a roughened surface of an implant is surrounded by bone regardless of the implant design.