-
0
Patient Assessment
- 0.1 Patient Demand
- 0.2 Anatomical location
-
0.3
Patient History
- 2.1 General patient history
- 2.2 Local history
-
0.4
Risk Assessment
- 3.1 Risk Assessment Overview
- 3.2 Age
- 3.3 Patient Compliance
- 3.4 Smoking
- 3.5 Drug Abuse
- 3.6 Recreational Drug and Alcohol Abuse
- 3.7 Condition of Natural Teeth
- 3.8 Parafunctions
- 3.9 Diabetes
- 3.10 Anticoagulants
- 3.11 Osteoporosis
- 3.12 Bisphosphonates
- 3.13 MRONJ
- 3.14 Steroids
- 3.15 Radiotherapy
- 3.16 Risk factors
-
1
Diagnostics
-
2
Treatment Options
-
2.1
Treatment planning
- 0.1 Non-implant based treatment options
- 0.2 Treatment planning conventional, model based, non-guided, semi-guided
- 0.3 Digital treatment planning
- 0.4 NobelClinician and digital workflow
- 0.5 Implant position considerations overview
- 0.6 Soft tissue condition and morphology
- 0.7 Site development, soft tissue management
- 0.8 Hard tissue and bone quality
- 0.9 Site development, hard tissue management
- 0.10 Time to function
- 0.11 Submerged vs non-submerged
- 0.12 Healed or fresh extraction socket
- 0.13 Screw-retained vs. cement-retained
- 0.14 Angulated Screw Channel system (ASC)
- 2.2 Treatment options esthetic zone
- 2.3 Treatment options posterior zone
- 2.4 Comprehensive treatment concepts
-
2.1
Treatment planning
-
3
Treatment Procedures
-
3.1
Treatment procedures general considerations
- 0.1 Anesthesia
- 0.2 peri-operative care
- 0.3 Flap- or flapless
- 0.4 Non-guided protocol
- 0.5 Semi-guided protocol
- 0.6 Guided protocol overview
- 0.7 Guided protocol NobelGuide
- 0.8 Parallel implant placement considerations
- 0.9 Tapered implant placement considerations
- 0.10 3D implant position
- 0.11 Implant insertion torque
- 0.12 Intra-operative complications
- 0.13 Impression procedures, digital impressions, intraoral scanning
- 3.2 Treatment procedures esthetic zone surgical
- 3.3 Treatment procedures esthetic zone prosthetic
- 3.4 Treatment procedures posterior zone surgical
- 3.5 Treatment procedures posterior zone prosthetic
-
3.1
Treatment procedures general considerations
-
4
Aftercare
Diagnostic imaging overview
Key points
- Diagnostic imaging is often an essential element in oral rehabilitation for a missing single tooth.
- Intra-oral imaging is often sufficient to establish a proper evaluation of the bone and neighbouring teeth.
- Cross-sectional imaging may be relevant to assess remaining bone volume and anatomical landmarks in the vicinity.
- Three-dimensional imaging opened the possibility for preoperative implant planning and guided surgery.
Introduction
Diagnostic imaging is an important element of the treatment planning in oral rehabilitation of a missing single tooth.
There should be no imaging prior to a thorough clinical examination. One should consider cost and radiation issues prior to choosing the appropriate imaging technique. When a removable denture is planned to replace a missing single tooth, there is no apparent justification to radiograph the edentulous space in the absence of clinical signs or symptoms. When a fixed denture is planned intra-oral radiographs of the abutment teeth should be taken to assess the periapical region and dental and periodontal structures. Using supplementary cross-sectional imaging should only be done after conventional radiography has been evaluated and judged insufficient. Spiral computerized tomography (CT) leads to an increased radiation vs. cone beam CT (CBCT).
3D Imaging
The greatest benefits of the 3D imaging are:
- the ability to analyze the anatomy of the patient’s jaw volume before surgery,
- identify vital structures, such as adjacent root positions, nerve canal, sinus wall, cortical borders,
- being free from errors introduced by poorly positioned films,
- the placement of implants without bone grafting, like tilted implants or short implants.
The 3D visualization of the features of implant recipient sites and anatomy often influences the surgical and prosthetic decision making.
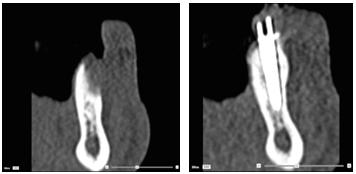
Figures 1 & 2: CT scans taken before (left) and after (right) implant placement and guided bone reconstruction.
Guided Surgery
Computer-assisted template-based implant planning and placement require the need for cross-sectional imaging.
Most guided surgery systems also allow the visualization of the desired restorative outcome, in the form of a diagnostic tooth setup that is scanned and displayed fully correlated with the scan of the anatomy. This empowers the ideal placement from both bone and prosthetic considerations.
Guided-surgery opened the possibility for preoperative implant planning and proper communication with the patient, surgeon and the prosthodontist. One of the main advantages of computer-guided rehabilitation is less postoperative pain and swelling but such advantage could require higher biological cost. Medical exposure to ionizing radiation and associated risks must always be considered and result in a net benefit to the patient.
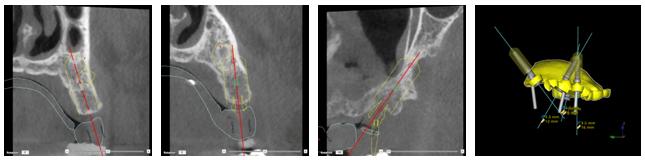
Figures 3-6: 3D implant planning and cross-sectional view (left 3 images), Surgical Guide (right)
Summary
The choice of the specific imaging technique appropriate for a given patient depends on the case, the different stage of treatment, and last but not least, the clinicians’ experience. However, the As Low As Reasonably Achievable (ALARA) principle must also be applied, taking into account any alternative techniques that might achieve the same diagnostic information required by the dental team.