-
0
Patient Assessment
- 0.1 Patient Demand
- 0.2 Anatomical location
-
0.3
Patient History
- 2.1 General patient history
- 2.2 Local history
-
0.4
Risk Assessment
- 3.1 Risk Assessment Overview
- 3.2 Age
- 3.3 Patient Compliance
- 3.4 Smoking
- 3.5 Drug Abuse
- 3.6 Recreational Drug and Alcohol Abuse
- 3.7 Condition of Natural Teeth
- 3.8 Parafunctions
- 3.9 Diabetes
- 3.10 Anticoagulants
- 3.11 Osteoporosis
- 3.12 Bisphosphonates
- 3.13 MRONJ
- 3.14 Steroids
- 3.15 Radiotherapy
- 3.16 Risk factors
-
1
Diagnostics
-
2
Treatment Options
-
2.1
Treatment planning
- 0.1 Non-implant based treatment options
- 0.2 Treatment planning conventional, model based, non-guided, semi-guided
- 0.3 Digital treatment planning
- 0.4 NobelClinician and digital workflow
- 0.5 Implant position considerations overview
- 0.6 Soft tissue condition and morphology
- 0.7 Site development, soft tissue management
- 0.8 Hard tissue and bone quality
- 0.9 Site development, hard tissue management
- 0.10 Time to function
- 0.11 Submerged vs non-submerged
- 0.12 Healed or fresh extraction socket
- 0.13 Screw-retained vs. cement-retained
- 0.14 Angulated Screw Channel system (ASC)
- 2.2 Treatment options esthetic zone
- 2.3 Treatment options posterior zone
- 2.4 Comprehensive treatment concepts
-
2.1
Treatment planning
-
3
Treatment Procedures
-
3.1
Treatment procedures general considerations
- 0.1 Anesthesia
- 0.2 peri-operative care
- 0.3 Flap- or flapless
- 0.4 Non-guided protocol
- 0.5 Semi-guided protocol
- 0.6 Guided protocol overview
- 0.7 Guided protocol NobelGuide
- 0.8 Parallel implant placement considerations
- 0.9 Tapered implant placement considerations
- 0.10 3D implant position
- 0.11 Implant insertion torque
- 0.12 Intra-operative complications
- 0.13 Impression procedures, digital impressions, intraoral scanning
- 3.2 Treatment procedures esthetic zone surgical
- 3.3 Treatment procedures esthetic zone prosthetic
- 3.4 Treatment procedures posterior zone surgical
- 3.5 Treatment procedures posterior zone prosthetic
-
3.1
Treatment procedures general considerations
-
4
Aftercare
Healed or fresh extraction socket
Key points
- Short term survival of implants placed in healed vs. fresh extraction sockets seems similar.
- Discrepancies in size between an extracted root and a more narrow immediately placed implant frequently require gaps to be filled with bone particles, aiming at bone site preservation.
- Long-term data on this subject are limited.
Introduction
Single-tooth implants are often immediately placed after extraction of incisors, canines and bicuspids. Careful tooth removal with preserved bone socket walls and infection control provide for such an approach, often with immediate or early loading. Extracted molars with 2-3 roots will leave a huge bone defect behind and a staged approach is commonly used. This is due to difficulties in obtaining primary implant stability, but also due to the shortage of soft tissue volume to cover a submerged implant. In short-term follow-up studies no difference between placing implants in fresh extraction sockets vs. healed sockets was found. Recent literature shows that immediate implant placement combined with immediate loading does also not decrease survival rates of implants.
Immediate implant placement in fresh extraction sockets cannot prevent resorption of the alveolar crest, albeit guided bone regeneration using bone substitutes and a collagen membrane may improve preservation of the alveolar ridge height and width. An advantage of immediate placement of implants is however the preservation to a certain extent of the peri-implant soft tissue. After 2 years peri-implant bone resorption rates of implants placed in fresh extraction vs. healed sockets are similar.
Implants in healed extraction sockets
Advantages:
- Resolution of possible infections
- Healing of bone defects
- Increased soft tissue volume generated by soft tissue healing of the extraction socket
Disadvantages:
- Progressive reduction of bone volume by continuing alveolar ridge resorption. May be partly counteracted by filling the alveolus with e.g. xenogenic bone particles
- Extended treatment time
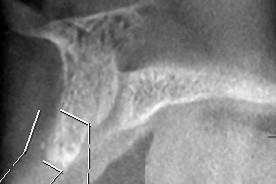
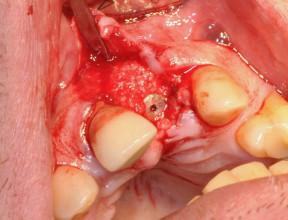
Figures 1 & 2: Root remnant in upper right central incisor position extracted. Figure 3: Alveolus filled with xenogenic bone and covered with a collagen membrane.
Figure 4: Radiograph obtained 6 months post extraction showing sufficient sagittal/vertical bone dimension. Figure 5: Placement of implant. Figure 6: Healing abutment connected 2 months post implant insertion.
Implants in fresh extraction sockets
Advantages:
- Reduction of total treatment time
- Reduction of patients’ discomfort
Disadvantages:
- Primary stability may be compromised
- Volume of keratinised mucosa on buccal/lingual site implant may be compromised
Figure 7: Root remnant in upper left central incisor position extracted. Figure 8: Immediate implant placement. Figure 9: Residual gap between implant and bone wall of alveolus filled with xenogenic bone. Figure 10: Covered with a collagen membrane.