-
0
Patient Assessment
- 0.1 Patient Demand
- 0.2 Anatomical location
-
0.3
Patient History
- 2.1 General patient history
- 2.2 Local history
-
0.4
Risk Assessment
- 3.1 Risk Assessment Overview
- 3.2 Age
- 3.3 Patient Compliance
- 3.4 Smoking
- 3.5 Drug Abuse
- 3.6 Recreational Drug and Alcohol Abuse
- 3.7 Condition of Natural Teeth
- 3.8 Parafunctions
- 3.9 Diabetes
- 3.10 Anticoagulants
- 3.11 Osteoporosis
- 3.12 Bisphosphonates
- 3.13 MRONJ
- 3.14 Steroids
- 3.15 Radiotherapy
- 3.16 Risk factors
-
1
Diagnostics
-
2
Treatment Options
-
2.1
Treatment planning
- 0.1 Non-implant based treatment options
- 0.2 Treatment planning conventional, model based, non-guided, semi-guided
- 0.3 Digital treatment planning
- 0.4 NobelClinician and digital workflow
- 0.5 Implant position considerations overview
- 0.6 Soft tissue condition and morphology
- 0.7 Site development, soft tissue management
- 0.8 Hard tissue and bone quality
- 0.9 Site development, hard tissue management
- 0.10 Time to function
- 0.11 Submerged vs non-submerged
- 0.12 Healed or fresh extraction socket
- 0.13 Screw-retained vs. cement-retained
- 0.14 Angulated Screw Channel system (ASC)
- 2.2 Treatment options esthetic zone
- 2.3 Treatment options posterior zone
- 2.4 Comprehensive treatment concepts
-
2.1
Treatment planning
-
3
Treatment Procedures
-
3.1
Treatment procedures general considerations
- 0.1 Anesthesia
- 0.2 peri-operative care
- 0.3 Flap- or flapless
- 0.4 Non-guided protocol
- 0.5 Semi-guided protocol
- 0.6 Guided protocol overview
- 0.7 Guided protocol NobelGuide
- 0.8 Parallel implant placement considerations
- 0.9 Tapered implant placement considerations
- 0.10 3D implant position
- 0.11 Implant insertion torque
- 0.12 Intra-operative complications
- 0.13 Impression procedures, digital impressions, intraoral scanning
- 3.2 Treatment procedures esthetic zone surgical
- 3.3 Treatment procedures esthetic zone prosthetic
- 3.4 Treatment procedures posterior zone surgical
- 3.5 Treatment procedures posterior zone prosthetic
-
3.1
Treatment procedures general considerations
-
4
Aftercare
Biologic complications
Key points
- Biologic complications are often caused by infection. Implants should be inserted in sites free of infection.
- Excess of cement may induce inflammation and marginal bone loss.
- Implants are occasionally lost because of occlusal overload.
- Implant-supported single-crowns may show infra-positioning after years of function.
Biologic complications
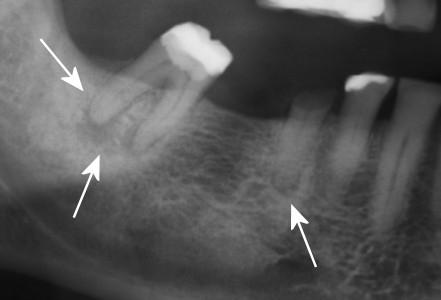
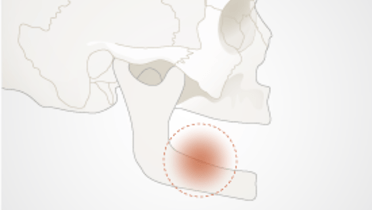
Extraction of teeth with persistent periapical lesions requires a specific drilling protocol to remove infected bone, to reach healthy trabecular bone and start up a bleeding. Residual dens sclerotic bone may harbor latent pathogenic microorganisms for a long period of time, which may later cause acute infection around an inserted implant.
Figures 1-2: Sclerotic bone enclosing periapical lesions (white arrows). Acute apical peri-implant lesion (yellow arrows)
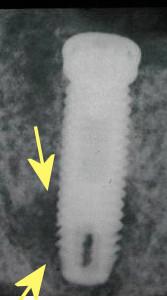
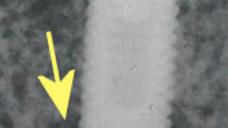
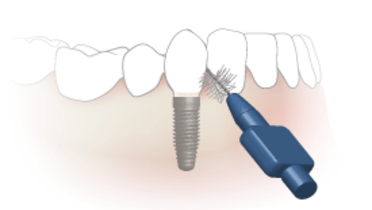
Single implant-supported crowns have frequently been cemented because of unfavorable implant directions, thus eliminating access-holes in the esthetic zone. Excess of cement is a common finding, causing inflammation and sometimes marginal bone loss. Careful removal of cement remnants is strongly advised. Today the problem can be avoided with screw retained crowns for all situations, using angulated screw channel abutments.
Figures 3-4: Remnants of cement causing marginal bone resorption (white arrows). Bone regeneration after cement removal (yellow arrow)
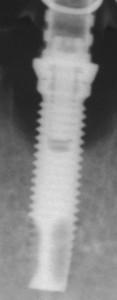
Marginal bone loss of ≥2 mm compared to initial radiographs (at suprastructure installation or within the first 3 months) associated with bleeding on probing should lead to further examinations, including repeated radiographs to confirm or invalidate the suspicion of peri-implantitis. The diagnosis is based on suppuration, deepening of the pockets around the implant and progressive marginal bone loss.
Different treatment strategies are suggested: only 1-2% of implant patients effectively need peri-implantitis surgery. For the decontamination of the infected implant surface, rinsing with saline, cleaning with cotton pellets with saline, mechanical debridement, Er:YAG laser treatment all seem equally efficient. Implantoplasty through open flap surgery can also be performed. When advanced marginal bone loss is observed, even revision surgery with replacement of the implant should be considered.
Figures 5-8: Progressive crater-shaped marginal bone loss with recurrent swelling, pain, pus/bleeding on probing. Implant with surrounding bone removed with a trephine drill
Implant-supported single-crowns may often show signs of infra-positioning after years in function, as a result of continuous eruption of teeth. This phenomenon has been described also for older age-groups with completed body growth. Not infrequently there is a need for remaking the crown.
Figures 9-10: Infra-position of upper right central incisor (arrows) after 15 years in function. Continuous eruption of adjacent teeth
Occasionally an implant becomes mobile without clear signs of infection. The radiographic image is quite typical showing a thin zone of osteolysis lining the whole periphery of the implant. Occlusal overload is claimed to be the cause.
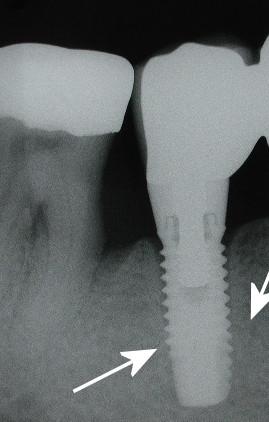
Figure 11: Osteolysis around the whole periphery (arrows) causing implant mobility