-
0
Patient Assessment
- 0.1 Patient Demand
- 0.2 Anatomical location
-
0.3
Patient History
- 2.1 General patient history
- 2.2 Local history
-
0.4
Risk Assessment
- 3.1 Risk Assessment Overview
- 3.2 Age
- 3.3 Patient Compliance
- 3.4 Smoking
- 3.5 Drug Abuse
- 3.6 Recreational Drug and Alcohol Abuse
- 3.7 Condition of Natural Teeth
- 3.8 Parafunctions
- 3.9 Diabetes
- 3.10 Anticoagulants
- 3.11 Osteoporosis
- 3.12 Bisphosphonates
- 3.13 MRONJ
- 3.14 Steroids
- 3.15 Radiotherapy
- 3.16 Risk factors
-
1
Diagnostics
-
2
Treatment Options
-
2.1
Treatment planning
- 0.1 Non-implant based treatment options
- 0.2 Treatment planning conventional, model based, non-guided, semi-guided
- 0.3 Digital treatment planning
- 0.4 NobelClinician and digital workflow
- 0.5 Implant position considerations overview
- 0.6 Soft tissue condition and morphology
- 0.7 Site development, soft tissue management
- 0.8 Hard tissue and bone quality
- 0.9 Site development, hard tissue management
- 0.10 Time to function
- 0.11 Submerged vs non-submerged
- 0.12 Healed or fresh extraction socket
- 0.13 Screw-retained vs. cement-retained
- 0.14 Angulated Screw Channel system (ASC)
- 2.2 Treatment options esthetic zone
- 2.3 Treatment options posterior zone
- 2.4 Comprehensive treatment concepts
-
2.1
Treatment planning
-
3
Treatment Procedures
-
3.1
Treatment procedures general considerations
- 0.1 Anesthesia
- 0.2 peri-operative care
- 0.3 Flap- or flapless
- 0.4 Non-guided protocol
- 0.5 Semi-guided protocol
- 0.6 Guided protocol overview
- 0.7 Guided protocol NobelGuide
- 0.8 Parallel implant placement considerations
- 0.9 Tapered implant placement considerations
- 0.10 3D implant position
- 0.11 Implant insertion torque
- 0.12 Intra-operative complications
- 0.13 Impression procedures, digital impressions, intraoral scanning
- 3.2 Treatment procedures esthetic zone surgical
- 3.3 Treatment procedures esthetic zone prosthetic
- 3.4 Treatment procedures posterior zone surgical
- 3.5 Treatment procedures posterior zone prosthetic
-
3.1
Treatment procedures general considerations
-
4
Aftercare
Digital treatment planning overview
Key points
- Virtual placement of implants allows to identify and fully use available bone volume, to optimize implant placement according to the approved prosthetic design.
- Since anatomical structures are revealed, damage to adjacent roots, sinus membrane, nerves and vessels can be better prevented.
- Digital treatment using dedicate software allows for preoperative implant planning and proper communication with the patient, surgeon, prosthodontist and dental technician.
One of the fastest growing fields of implant dentistry is the utilization of computer tomography (CT) scan data and treatment planning software in conjunction with guided surgery for implant cases. Treatment planning for implant placement has evolved from a purely surgical approach strictly focused on bone availability, into a truly restoratively-driven planning approach using computer-guided templates.
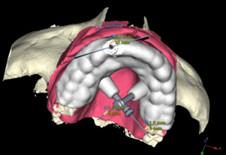
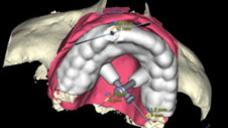
Cone Beam computer tomography (CBCT) or CT data-sets of the patient jaw bones are combined with a scan of the patient’s ideal model and the restorative outcome to produce three-dimensional (3D) images of the jaw bones, the desired restoration and thickness of the mucosa. Software planning can be made in a full 3D data set (or in more familiar 2D and then recalculated to produce 3D images). Planning in full 3D mode allows the clinician to choose any viewpoint in the virtual reality, avoids recalculations of the data set and renders planning more intuitively, since it is similar to the real world.
The approved prosthetic design of the tooth to be replaced is scanned and imported into the digital plan, allowing the clinician to relate the restoration with the patient’s available soft and hard tissues, from both prosthetic and surgical perspectives. The scanned restoration helps to visualize the optimal prosthetic outcome, therefore, implant position can be optimized according to the esthetic and functional needs, when the available bone allows for it. Matching the position and inclination of implants towards the prosthesis is a major advantage of 3-D planning both biomechanically and esthetically. Furthermore, an interim prosthesis can be manufactured prior to the surgical procedure, allowing for an immediate function.
The most popular and certified implant treatment planning and guided surgery systems available on the market is NobelClinician® (Nobel Biocare, AG). Today, integrated digital work-flow allows full integration of therapeutic steps from patient diagnostics and treatment planning to surgery and prosthetic design. For instance, NobelClinician software combines the data from CBCT patient scan with the 2G NobelProcera scan (Nobel Biocare, AG) of the model & wax-up into a single surgical and esthetic view. This protocol greatly simplifies the overall treatment workflow while providing an enhanced fit of the surgical guide to the patient. Partial and single cases may take advantages from this new technology in term of simplicity, accuracy, and lower costs.
Anatomical structures and safety zones
The images reveal height, width and trabecular/cortical structure of available bone allowing for optimal implant placement. Mucosa thickness, location of the maxillary sinuses, mandibular canal, mental foramen and incisive canal all have to be considered in the planning. A safety zone towards anatomical structures should be respected since deviations from anatomical reality can occur during imaging, software data transformation and surgery. These deviations can add up and become clinically relevant. The clinician should clearly elaborate with the commercial company involved how large this safety zone should be, based on the maximum deviation observed in their clinical reports. NobelClinician Software is the most certified software. The reported deviation from planned to placed implants were less then the safety zone. Furthermore, Tooth-supported templates provide more accurate results than mucosa-supported templates.
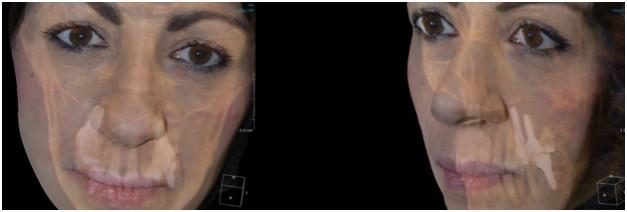
Computer-aided design/computer-aided manufacturing (CAD/CAM)-processed surgical guides are easily obtained from the same image data set. One can choose between guided pilot drilling or for fully guided surgery. Even when no surgical templates are fabricated, the visual transfer of the planning to the operative field improves precision of reproducing the planning and reduces surgery time. Software which integrates the extraoral face scan allow to further optimize esthetics.
Finally, the treatment planning can be shared through the internet among the team members including the laboratory technician allowing for interactive and interdisciplinary planning. The data set of the planned prosthesis can be used for its preoperative manufacturing through the CAD/CAM technology. It can also be sent to an expert for a second opinion. The treatment planning can be shown to the patient, even fusing the radiological data with clinical images to improve understanding of what is at stake and improve acceptance through 3D visualization.
Figures 1a & 1b: Face and soft tissue analysis performed by the superimposition of the CBCT scan and a three-dimensional pictures.
Figures 2 & 3: Diagnostic images Figure 4: Virtual Surgical Template
Figures 5-7: 3.0mm implant placed and immediately loaded