-
0
Patient Assessment
- 0.1 Patient Demand
- 0.2 Anatomical location
-
0.3
Patient History
- 2.1 General patient history
- 2.2 Local history
-
0.4
Risk Assessment
- 3.1 Risk Assessment Overview
- 3.2 Age
- 3.3 Patient Compliance
- 3.4 Smoking
- 3.5 Drug Abuse
- 3.6 Recreational Drug and Alcohol Abuse
- 3.7 Condition of Natural Teeth
- 3.8 Parafunctions
- 3.9 Diabetes
- 3.10 Anticoagulants
- 3.11 Osteoporosis
- 3.12 Bisphosphonates
- 3.13 MRONJ
- 3.14 Steroids
- 3.15 Radiotherapy
- 3.16 Risk factors
-
1
Diagnostics
-
2
Treatment Options
-
2.1
Treatment planning
- 0.1 Non-implant based treatment options
- 0.2 Treatment planning conventional, model based, non-guided, semi-guided
- 0.3 Digital treatment planning
- 0.4 NobelClinician and digital workflow
- 0.5 Implant position considerations overview
- 0.6 Soft tissue condition and morphology
- 0.7 Site development, soft tissue management
- 0.8 Hard tissue and bone quality
- 0.9 Site development, hard tissue management
- 0.10 Time to function
- 0.11 Submerged vs non-submerged
- 0.12 Healed or fresh extraction socket
- 0.13 Screw-retained vs. cement-retained
- 0.14 Angulated Screw Channel system (ASC)
- 2.2 Treatment options esthetic zone
- 2.3 Treatment options posterior zone
- 2.4 Comprehensive treatment concepts
-
2.1
Treatment planning
-
3
Treatment Procedures
-
3.1
Treatment procedures general considerations
- 0.1 Anesthesia
- 0.2 peri-operative care
- 0.3 Flap- or flapless
- 0.4 Non-guided protocol
- 0.5 Semi-guided protocol
- 0.6 Guided protocol overview
- 0.7 Guided protocol NobelGuide
- 0.8 Parallel implant placement considerations
- 0.9 Tapered implant placement considerations
- 0.10 3D implant position
- 0.11 Implant insertion torque
- 0.12 Intra-operative complications
- 0.13 Impression procedures, digital impressions, intraoral scanning
- 3.2 Treatment procedures esthetic zone surgical
- 3.3 Treatment procedures esthetic zone prosthetic
- 3.4 Treatment procedures posterior zone surgical
- 3.5 Treatment procedures posterior zone prosthetic
-
3.1
Treatment procedures general considerations
-
4
Aftercare
Implant selection and drill protocols, posterior zone
Key points
- Make the right implant diameter selection.
- Make the right implant number selection.
- Accurate plan may avoid implant bone resorption and soft tissue recession.
Implant placement requires an adequate quantity and quality of bone. Following tooth extraction residual alveolar ridge resorbs. The amount of horizontal bone loss is generally the greatest and occurs more frequently on the buccal side. The anatomical limitations of residual alveolar bone can limit the insertion of an aesthetically ideal and functional dental implants.
Bone Quantity and Density
The selection of the ideal number of implants is related to the bone volume and density. The low-density and quantity of bone and the presence of sinus pneumatization in maxilla are relevant anatomic characteristics in the posterior region, since they can limit the implant height. In the posterior region of upper jaw, it is recommended to insert 3 implants to replace 3 missing teeth. Maintaining adequate distance from adjacent teeth also helps preserve crestal bone and interproximal papillary height.
The mandibular canal is an important structure that could limit the installation of dental implants in lower jaws. According to Jivraj et al. and Vazquez et al., a distance of at least 2 mm between the most apical part of the implant and vascular and neurologic structures must be respect. The lingual mandibular bone concavity is another important factor since it increases the risks of fenestrations or perforations during implant insertion, in case of deficient buccal-lingual angulation. The mental foramen is an important mandibular structure when placing implants in the foraminal region.
The localization of the mandibular canal, the submandibular fossa, and the maxillary sinuses, in addition to the angulation of the alveolar crest and the bone volume, are of primary importance during implant treatment planning in the posterior jaw area. Therefore, the use of CT in all sliced images is suggested to indicate the most convenient dimensions of the implant and its optimal position and inclination.
Implant Selection, Length and Diameter
The selection of the ideal number of implants is highly dependent on the amount and quality of the available bone, as well as adjacent anatomy. To obtain excellent results with dental implants, meticulous attention must be paid to details. Additionally, the posterior quadrants of the mouth are challenging for dental implants due to their anatomical and occlusal features. The mesiodistal space required for placing an implant is related to the type and number of teeth that will be replaced. According to Misch, the selection of implant size is influenced by the mesiodistal distance available for implant placement. These authors indicated a guideline for this selection: a distance of at least 1.5 mm must be respected between the implant and the adjacent teeth; a distance of at least 3.0 mm between the implant and an adjacent implant.
Immediate placement of dental implants into mandibular molar sockets has also been presented as a successful alternative to the delayed protocol. An essential factor for successful immediate implant placement is initial stabilization of the implant with the apical and/or lateral bone. In molar extraction sockets, achieving initial implant stability may be challenging as a result of the width of the alveolar socket, poor bone quality, and anatomical limitations beyond the apices of molar roots, such as the inferior alveolar nerve, as well as the maxillary sinus.
Increased mechanical stability and bone-implant contact are achieved using implants with a large diameter (from 5.0 up to 6.0 mm). Therefore, wide-diameter implants (5 mm or more) should take advantage of bone width, reducing the gap between the post-extractive socket, increasing the surface available for osseointegration, and reaching primary stability not typically achieved with a standard-diameter implants. In addition, their use provide an effective counter acting occlusal force of the magnitude that may be observed in molar areas. Finally, the wide-diameter implants mimic the emergence profile of the molar tooth.
In the posterior maxilla, tooth loss is usually associated with alveolar bone resorption and sinus pneumatization. In addition, the poor bone quality of the posterior maxilla has a negative influence on the survival rate of implants placed in the maxillary posterior sextants. Therefore, the treatment planning of the atrophic posterior maxilla for implant placement remains various, with the dilemma of whether to place short implants (4 to 6 mm), tilted implants or to augment the floor of the maxillary sinus. Short implants can be successfully loaded in maxillary bone with a residual height of 4 to 6 mm, but their long-term prognosis is unknown, thus long-term, stronger evidence is needed to confirm this preliminary finding.
Internal or External connection
The reduced marginal bone loss experienced with platform switched, conical connection implants may be of importance in areas of aesthetic concern, as well as in the posterior zone, reducing the risk of an exposed metal implant shoulder and/ or reducing the distance between the nearest teeth/ implants.
Drill Protocols, Posterior Zone
The root-form implant design with a variable- threaded geometry, and a moderately rough surface facilitate the one-stage surgical procedures and in order to allow for immediate placement and anticipated loading protocols. The osteotome effect of the tapered implant body design improves the likelihood of adequate primary stability needed to ensure immediate implant placement and loading.
Various adaptations to clinical procedures have been proposed, including the under-preparation of the implant site (maxilla) to achieve high primary stability even in poor bone.
Irrigation and Thermal Osteonecrosis
Failure of dental implants may be attributed to both endogenous and exogenous factors. Excessive surgical trauma related to the surgical technique, can be responsible for implant failure. It is known that rises in bone temperature during rotary instrumentation is expected to rise as a function of the amount of pressure and cutting necessary for site preparation and the effectiveness of cooling irrigation. Thermal osteonecrosis is inexorable if the bone temperature rises higher than 47°C. This has been reported clinically to be one of the causes of implant periapical lesions.
To avoid thermal osteonecrosis, copious cooling irrigation, new drills, recommended speed drilling, and respect of the guidelines for the implant site preparation, according to the bone density, are prerequisite for implant success. Some authors have proposed to avoid drilling sequence in favor of an osteotome technique. However, this could be less precise in implant position and could be not comfortable for patients.
Guided Implant Placement
Single implants placed using computer-assisted template based surgery are associated with higher accuracy, compared to single implants placed using surgical navigation system. Avoidance of critical anatomic structures, the aesthetic and functional advantages of prosthodontic-driven implant positioning must also be considered.
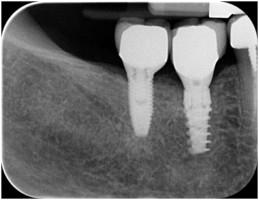
Figure 1 Figure 2 External hex versus conical connection implants in the posterior area
Figure 3 Figure 4
Figure 5 Figure 6 Figures 3-6: Wide-diameter implants and CAD/CAM technologies to replace a molar (1 year follow-up)