-
0
Patient Assessment
- 0.1 Patient Demand
- 0.2 Anatomical location
-
0.3
Patient History
- 2.1 General patient history
- 2.2 Local history
-
0.4
Risk Assessment
- 3.1 Risk Assessment Overview
- 3.2 Age
- 3.3 Patient Compliance
- 3.4 Smoking
- 3.5 Drug Abuse
- 3.6 Recreational Drug and Alcohol Abuse
- 3.7 Condition of Natural Teeth
- 3.8 Parafunctions
- 3.9 Diabetes
- 3.10 Anticoagulants
- 3.11 Osteoporosis
- 3.12 Bisphosphonates
- 3.13 MRONJ
- 3.14 Steroids
- 3.15 Radiotherapy
- 3.16 Risk factors
-
1
Diagnostics
-
2
Treatment Options
-
2.1
Treatment planning
- 0.1 Non-implant based treatment options
- 0.2 Treatment planning conventional, model based, non-guided, semi-guided
- 0.3 Digital treatment planning
- 0.4 NobelClinician and digital workflow
- 0.5 Implant position considerations overview
- 0.6 Soft tissue condition and morphology
- 0.7 Site development, soft tissue management
- 0.8 Hard tissue and bone quality
- 0.9 Site development, hard tissue management
- 0.10 Time to function
- 0.11 Submerged vs non-submerged
- 0.12 Healed or fresh extraction socket
- 0.13 Screw-retained vs. cement-retained
- 0.14 Angulated Screw Channel system (ASC)
- 2.2 Treatment options esthetic zone
- 2.3 Treatment options posterior zone
- 2.4 Comprehensive treatment concepts
-
2.1
Treatment planning
-
3
Treatment Procedures
-
3.1
Treatment procedures general considerations
- 0.1 Anesthesia
- 0.2 peri-operative care
- 0.3 Flap- or flapless
- 0.4 Non-guided protocol
- 0.5 Semi-guided protocol
- 0.6 Guided protocol overview
- 0.7 Guided protocol NobelGuide
- 0.8 Parallel implant placement considerations
- 0.9 Tapered implant placement considerations
- 0.10 3D implant position
- 0.11 Implant insertion torque
- 0.12 Intra-operative complications
- 0.13 Impression procedures, digital impressions, intraoral scanning
- 3.2 Treatment procedures esthetic zone surgical
- 3.3 Treatment procedures esthetic zone prosthetic
- 3.4 Treatment procedures posterior zone surgical
- 3.5 Treatment procedures posterior zone prosthetic
-
3.1
Treatment procedures general considerations
-
4
Aftercare
Implant selection and drill protocols, anterior
Key points
- Make the right implant diameter selection.
- Make the right implant number selection.
- Accurate plan may avoid implant bone resorption and soft tissue recession.
The essential prerequisites for an optimally esthetic implant restoration should always remain a careful, precise, comprehensive, biologically- and prosthetically-based diagnosis, as well as the choice of the most appropriate, most conservative, and least traumatic treatment techniques, aimed at conserving, and where necessary augmenting gingival and bone to achieve a successful outcome. Advances in surgical techniques and implant materials have moved implant treatment beyond mere functional integration towards restoratively driven principles, with a heightened awareness that favorable results will largely depend on biologically driven therapy.
Looking into the literature, single-tooth replacement by means of osseointegrated dental implants may be considered a reliable treatment option to replace missing teeth, following both immediate and early protocols. These rehabilitations offer substantial benefits when compared with removable partial dentures, such as improved occlusion and support, simplification of the prosthesis, less invasive restorative procedures, bone maintenance, and improvement in oral health impact.
The mesiodistal space required for placing an implant is related to the type and number of teeth that will be replaced. According to Misch, the selection of implant size is influenced by the mesiodistal distance available for implant placement. These authors indicated a guideline for this selection: a distance of at least 1.5 mm must be respected between the implant and the adjacent teeth; a distance of at least 3.0 mm between the implant and an adjacent implant. On the other hand, especially in cases where endogenous factors are not present, failure of dental implants has also been attributed to exogenous factors such as excessive surgical trauma related to the surgical technique.
Implant installation specially in narrow ridge and in aesthetic area should be performed very carefully and always respecting the ideal prosthetic guided implant position and the sufficient amount of bone volumes. Consequently implant placement and restoration of compromised alveolar ridges in the aesthetic zone has always been a challenge to the oral implantologists.
Bone Quantity and Density
Implant placement and restoration of compromised alveolar ridges in the aesthetic zone has always been a challenge to the oral surgeon. To achieve a successful esthetic result and good patient satisfaction, implant placement in the esthetic zone demands a thorough understanding of anatomic, biologic, surgical, and prosthetic principles. Very often the scenario of deficient and compromised anterior ridges is present and required extensive ridge augmentation before or concomitant to the implant placement. Drills should be used carefully with abundant irrigation to avoid bone damage. Alternatively, the use of bone expanders and bone condensers without the use of traditional drilling sequences in this scenario is becoming popular because of its predictable results. Viceversa, guided bone reconstruction procedures have to be associated with implant installation.
Implant Selection, Esthetic Zone
The selection of the ideal number of implants is highly dependent on the amount and quality of the available bone, as well as adjacent anatomy. This is particularly relevant in the anterior, esthetic zone. Understanding the bone anatomy, combined with implementing the proper drilling protocols greatly increases the odds for an esthetically pleasing outcome.
In the esthetic zone it is more predictable to place implants away from each other so that the intervening soft tissue can be sculpted to give the illusion of papilla, maintaining adequate distance from adjacent teeth also helps preserve crestal bone and interproximal papillary height.
Implant Diameter
Small-diameter implant (3 mm), and the platform-switching concept were used in a space of limited mesiodistal dimension. Narrow diameter dental implants have a good track record. Five-year studies show a success rate ranging from 91.2% to 96.3%. Narrow diameter dental implants have been gaining in popularity with clinicians as another means to rehabilitate patients with predictable results. Advantages include less invasive surgery, less post-operative discomfort, and good initial stability, which can make immediate loading possible, preserving and compressing patient’s bone, and conserving the gingival architecture.
Excellent bone levels were noted around the implant, and importantly, with no adverse effect on marginal bone levels on the adjacent teeth.
Implant Length
Longer implant should be used to improve the primary implant stability in cases of post-extractive fashion and if an immediate loading procedure has been planned. Adjacent tooth roots, amount of bone height, nerves, blood vessels, bicortical stabilization should be accurately evaluated before implant placement.
Internal or External connection
The reduced marginal bone loss experienced with platform switched, conical connection implants may be of importance in areas of aesthetic concern, eventually reducing the risk of an exposed metal implant shoulder and/ or reducing the distance between the nearest teeth/ implants.
Drill Protocols, Esthetic Zone
Recently, new implant designs and surfaces have been introduced to decrease the risk of early failure of immediately loaded implants. Various adaptations to clinical procedures have been proposed, including the under-preparation of the implant site to achieve high primary stability even in poor bone.
The root-form implant design with a variable-threaded geometry and a moderately rough surface has been introduced to facilitate the one-stage surgical procedures and in order to allow for immediate placement and anticipated loading protocols. The osteotome effect of the tapered implant body design improves the likelihood of adequate primary stability needed to ensure immediate implant placement and loading.
Primary stability can be improved by using a tapered implant in a slightly underprepared implant site.
Irrigation and Thermal Osteonecrosis
Failure of dental implants may be attributed to endogenous factors. Nevertheless, also exogenous factors, such as excessive surgical trauma related to the surgical technique, can be responsible for implant failure. It is known that rises in bone temperature during rotary instrumentation is expected to rise as a function of the amount of pressure and cutting necessary for site preparation and the effectiveness of cooling irrigation.F Thermal osteonecrosis is inexorable if the bone temperature rises higher than 47°C. This has been reported clinically to be one of the causes of implant periapical lesions. If elimination of the drilling sequence prevents excessive bone loss and wash out of growth factors which helps in regeneration. Abstaining from drilling also prevents heat generation thereby avoiding bone necrosis and also aid in decreasing the healing duration of the site, otherwise osteotome technique could be less precise in implant position and could be annoying for patients.
Guided Implant Placement
Single implants placed using computer-assisted template based surgery are associated with higher accuracy, compared to single implants placed using navigation system. Tooth-supported templates provide more accurate results than mucosa-supported templates. Thus results for this indication, are superior to those from complete edentulism. Avoidance of critical anatomic structures, aesthetic and functional advantages of prosthodontic-driven implant positioning must also be considered.
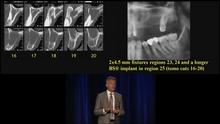
Figure 1 Figure 2
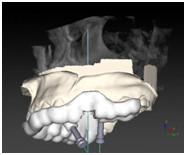
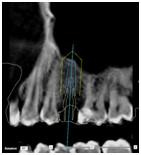
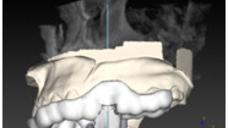
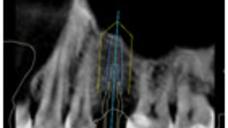
Figure 3 Figure 4
Figures 1-4: Two-year follow-up of NobelActive 3.0 implants (3.0 x 11.5 mm)
Figure 5 Figure 6 Figure 7 Figure 8

Figure 9 Figures 5-9: Single-guided (Nobel Clinician) implant placement (Osstem TSIII 4 x 11.5 mm).