-
0
Patient Assessment
- 0.1 Patient Demand
- 0.2 Anatomical location
-
0.3
Patient History
- 2.1 General patient history
- 2.2 Local history
-
0.4
Risk Assessment
- 3.1 Risk Assessment Overview
- 3.2 Age
- 3.3 Patient Compliance
- 3.4 Smoking
- 3.5 Drug Abuse
- 3.6 Recreational Drug and Alcohol Abuse
- 3.7 Condition of Natural Teeth
- 3.8 Parafunctions
- 3.9 Diabetes
- 3.10 Anticoagulants
- 3.11 Osteoporosis
- 3.12 Bisphosphonates
- 3.13 MRONJ
- 3.14 Steroids
- 3.15 Radiotherapy
- 3.16 Risk factors
-
1
Diagnostics
-
2
Treatment Options
-
2.1
Treatment planning
- 0.1 Non-implant based treatment options
- 0.2 Treatment planning conventional, model based, non-guided, semi-guided
- 0.3 Digital treatment planning
- 0.4 NobelClinician and digital workflow
- 0.5 Implant position considerations overview
- 0.6 Soft tissue condition and morphology
- 0.7 Site development, soft tissue management
- 0.8 Hard tissue and bone quality
- 0.9 Site development, hard tissue management
- 0.10 Time to function
- 0.11 Submerged vs non-submerged
- 0.12 Healed or fresh extraction socket
- 0.13 Screw-retained vs. cement-retained
- 0.14 Angulated Screw Channel system (ASC)
- 2.2 Treatment options esthetic zone
- 2.3 Treatment options posterior zone
- 2.4 Comprehensive treatment concepts
-
2.1
Treatment planning
-
3
Treatment Procedures
-
3.1
Treatment procedures general considerations
- 0.1 Anesthesia
- 0.2 peri-operative care
- 0.3 Flap- or flapless
- 0.4 Non-guided protocol
- 0.5 Semi-guided protocol
- 0.6 Guided protocol overview
- 0.7 Guided protocol NobelGuide
- 0.8 Parallel implant placement considerations
- 0.9 Tapered implant placement considerations
- 0.10 3D implant position
- 0.11 Implant insertion torque
- 0.12 Intra-operative complications
- 0.13 Impression procedures, digital impressions, intraoral scanning
- 3.2 Treatment procedures esthetic zone surgical
- 3.3 Treatment procedures esthetic zone prosthetic
- 3.4 Treatment procedures posterior zone surgical
- 3.5 Treatment procedures posterior zone prosthetic
-
3.1
Treatment procedures general considerations
-
4
Aftercare
Implant insertion torque
Key points
- The insertion torque is one objective measure that reflects the primary implant stability.
- The insertion torque value for a given jaw bone quality may be “manipulated” with the use of an adapted surgery technique.
- The insertion torque has a great impact on the chosen loading protocol, i.e. either one-stage surgery with early/immediate loading or two-stage surgery with a classic/prolonged healing period.
Definition
Total insertion torque (Ncm) reflects the consumed electric current during tapping or implant insertion by a motor unit-connected computer and is indirectly a value of the primary implant stability. The total insertion torque value is the sum of:
- the true cutting resistance of bone during tapping or implant insertion
- the friction
- the contribution of bone shiver packing in deeper preparations
Correlations have been shown between insertion torque values and:
- identified bone density assessed on radiographs of implant sites using an aluminum-reference
- assigned scores on preoperative radiographs according to a 1-4 bone quality classification
- resonance frequency values of primary implant stability obtained after insertion in maxillae and mandibles
Clinical implications
The insertion torque value is a result of the host jaw bone texture, drilling protocol, and implant design. An experienced implant surgeon can “manipulate” the insertion torque value to a certain extent by using an adapted surgery technique. Thus, one may either use a standard drilling protocol and adapt the implant design to the site in question (varies implant diameters or tapered implants) or one may instead adapt the drilling protocol (narrow/wide preparations) and use standard sized implants. An insertion torque of minimum 30 Ncm is regarded a prerequisite for one-stage surgery with early or immediate loading.
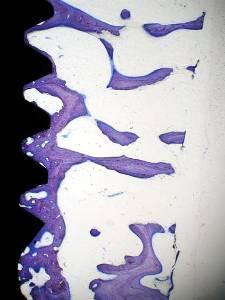
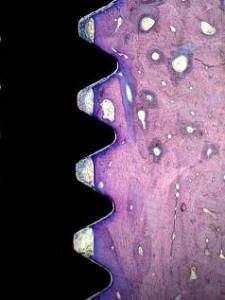
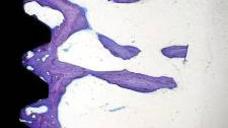
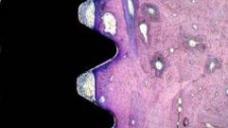
Figures 1: Implant placed in maxillary bone (right) and mandibular bone (left) presenting low and high insertion torque values, respectively. Courtesy of Professor Lars Sennerby, Göteborg, Sweden
Three major clinical signs of poor bone quality/poor implant stability may be identified during implant placement:
- despite a low pre-set motor torque (20 Ncm), the bone resistance may not bring about an automatic motor stop when the implant has reached its final position. Such an implant may still be kept in the bone site, albeit an extended healing period of 4 weeks is advocated, i.e. a total of 10-12 weeks of healing
- during cover screw tightening, the force exerted by the manual screw driver may be sufficient to rotate the implant as well. Such rotation mobility may be accepted and the implant can be kept in the bone site, albeit an extended healing period of 6 weeks is advocated, i.e. a total of 12-14 of healing
- an inserted implant may be moved either horizontally or vertically, indicating total implant mobility. Such an implant ought to be removed and preferably be replaced by a wider implant. As an alternative after removing the implant, a rongeur/bone scraper may be used for collecting bone shivers to be packed into the walls of the site, allowing the previously inserted implant to be reinserted and to encounter more resistance. Such an implant can be kept in the bone site, albeit an extended healing period of 8 weeks is advocated, i.e. a total of 14-16 weeks of healing