-
0
Patient Assessment
- 0.1 Patient Demand
- 0.2 Anatomical location
-
0.3
Patient History
- 2.1 General patient history
- 2.2 Local history
-
0.4
Risk Assessment
- 3.1 Risk Assessment Overview
- 3.2 Age
- 3.3 Patient Compliance
- 3.4 Smoking
- 3.5 Drug Abuse
- 3.6 Recreational Drug and Alcohol Abuse
- 3.7 Condition of Natural Teeth
- 3.8 Parafunctions
- 3.9 Diabetes
- 3.10 Anticoagulants
- 3.11 Osteoporosis
- 3.12 Bisphosphonates
- 3.13 MRONJ
- 3.14 Steroids
- 3.15 Radiotherapy
- 3.16 Risk factors
-
1
Diagnostics
-
2
Treatment Options
-
2.1
Treatment planning
- 0.1 Non-implant based treatment options
- 0.2 Treatment planning conventional, model based, non-guided, semi-guided
- 0.3 Digital treatment planning
- 0.4 NobelClinician and digital workflow
- 0.5 Implant position considerations overview
- 0.6 Soft tissue condition and morphology
- 0.7 Site development, soft tissue management
- 0.8 Hard tissue and bone quality
- 0.9 Site development, hard tissue management
- 0.10 Time to function
- 0.11 Submerged vs non-submerged
- 0.12 Healed or fresh extraction socket
- 0.13 Screw-retained vs. cement-retained
- 0.14 Angulated Screw Channel system (ASC)
- 2.2 Treatment options esthetic zone
- 2.3 Treatment options posterior zone
- 2.4 Comprehensive treatment concepts
-
2.1
Treatment planning
-
3
Treatment Procedures
-
3.1
Treatment procedures general considerations
- 0.1 Anesthesia
- 0.2 peri-operative care
- 0.3 Flap- or flapless
- 0.4 Non-guided protocol
- 0.5 Semi-guided protocol
- 0.6 Guided protocol overview
- 0.7 Guided protocol NobelGuide
- 0.8 Parallel implant placement considerations
- 0.9 Tapered implant placement considerations
- 0.10 3D implant position
- 0.11 Implant insertion torque
- 0.12 Intra-operative complications
- 0.13 Impression procedures, digital impressions, intraoral scanning
- 3.2 Treatment procedures esthetic zone surgical
- 3.3 Treatment procedures esthetic zone prosthetic
- 3.4 Treatment procedures posterior zone surgical
- 3.5 Treatment procedures posterior zone prosthetic
-
3.1
Treatment procedures general considerations
-
4
Aftercare
Soft tissue condition and morphology
Key points
- The establishment and maintenance of an efficient soft tissue seal around an implant as well as around a prosthetic framework are hallmarks for implant success.
- The existence of a physiological barrier underneath a implant-supported bridge restoration has been demonstrated.
- Treatment planning of classical restorative procedures and implants must take into account the periodontal biotype.
Once an implant is placed in function, peri-implant mucosal changes had been postulated as an attempt of the mucosal tissue to establish a stable biological dimension. If the thickness of peri-implant mucosa is reduced, bone resorption occurs to reestablish the mucosal dimension that was required for protection of the underlying tissues.
The influence of mucosal thickness and biologic width formation on tissue health maintenance and bone wall preservation around implants is today considered one of the most important concern for both function and esthetics. The term periodontal biotype was introduced by Seibert and Lindhe to describe the thickness of the gingiva in the faciopalatal dimension, and this is an important aspect in the maintenance of gingival health. It has been suggested the existence of a direct correlation between gingival biotype and the susceptibility to gingival recession around dental implants. Furthermore, the importance of the thickness of the alveolar ridge mucosa underneath a zirconia implant-supported restoration has been recently introduced, suggesting the existence of a physiological barrier underneath a implant-supported bridge restoration. These dimensions support the concept that the clinician may prepare the pontic recipient site in order to ensure an adequate mucosal thickness to properly house the prosthetic interface.
Although an objective classification of the gingival tissue thickness of different biotypes has not been defined, gingival biotype can be evaluated as follows:
- Direct visual assessment only;
- Visual assessment with the aid of a periodontal probe;
- Direct measurements, combining the previously methods;ef
- Measurements using the cone bean computer tomography.
Recently soft tissue cone-beam computed tomography combined with SmartFusion (Nobel Biocare, AG) technology is used to visualize, measure the dimensions, and analyze the relationship of several structures of the periodontium and dentogingival attachment apparatus. Furthermore, this method allow the determination of the dimensions and relationships of the structures of the dentogingival unit (figures).
Figure 1 Figure 2 Figure 3
Maxillary implant placement (Figure 1). Three years clinical (Figure 2) and radiographic view (Figure 3).
Figure 4 Figure 5 Figure 6 Mandibular implant placement (Figure 4). Three years clinical (Figure 5) and radiographic view (Figure 6)
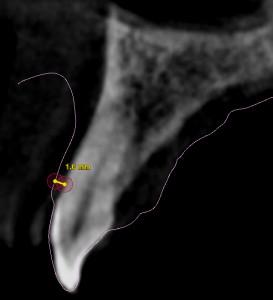
Figure 7: Measurement of the soft tissue thickness using SmartFusion technology