-
0
Patient Assessment
- 0.1 Patient Demand
- 0.2 Anatomical location
-
0.3
Patient History
- 2.1 General patient history
- 2.2 Local history
-
0.4
Risk Assessment
- 3.1 Risk Assessment Overview
- 3.2 Age
- 3.3 Patient Compliance
- 3.4 Smoking
- 3.5 Drug Abuse
- 3.6 Recreational Drug and Alcohol Abuse
- 3.7 Condition of Natural Teeth
- 3.8 Parafunctions
- 3.9 Diabetes
- 3.10 Anticoagulants
- 3.11 Osteoporosis
- 3.12 Bisphosphonates
- 3.13 MRONJ
- 3.14 Steroids
- 3.15 Radiotherapy
- 3.16 Risk factors
-
1
Diagnostics
-
2
Treatment Options
-
2.1
Treatment planning
- 0.1 Non-implant based treatment options
- 0.2 Treatment planning conventional, model based, non-guided, semi-guided
- 0.3 Digital treatment planning
- 0.4 NobelClinician and digital workflow
- 0.5 Implant position considerations overview
- 0.6 Soft tissue condition and morphology
- 0.7 Site development, soft tissue management
- 0.8 Hard tissue and bone quality
- 0.9 Site development, hard tissue management
- 0.10 Time to function
- 0.11 Submerged vs non-submerged
- 0.12 Healed or fresh extraction socket
- 0.13 Screw-retained vs. cement-retained
- 0.14 Angulated Screw Channel system (ASC)
- 2.2 Treatment options esthetic zone
- 2.3 Treatment options posterior zone
- 2.4 Comprehensive treatment concepts
-
2.1
Treatment planning
-
3
Treatment Procedures
-
3.1
Treatment procedures general considerations
- 0.1 Anesthesia
- 0.2 peri-operative care
- 0.3 Flap- or flapless
- 0.4 Non-guided protocol
- 0.5 Semi-guided protocol
- 0.6 Guided protocol overview
- 0.7 Guided protocol NobelGuide
- 0.8 Parallel implant placement considerations
- 0.9 Tapered implant placement considerations
- 0.10 3D implant position
- 0.11 Implant insertion torque
- 0.12 Intra-operative complications
- 0.13 Impression procedures, digital impressions, intraoral scanning
- 3.2 Treatment procedures esthetic zone surgical
- 3.3 Treatment procedures esthetic zone prosthetic
- 3.4 Treatment procedures posterior zone surgical
- 3.5 Treatment procedures posterior zone prosthetic
-
3.1
Treatment procedures general considerations
-
4
Aftercare
Implant design and implant selection
Key points
- In the event of limited mesiodistal width (lateral upper incisors, lower central incisors, [≤ 6 mm]), smaller-diameter implants (≤ 3.5 mm) are recommended.
- In the event of poor bone quality bone (D3-D4), longer implants are recommended when an immediate loading procedure is planned.
- Platform switching implants with a conical implant-abutment connection provides better results in terms of horizontal and vertical crestal bone loss, compared with flat to flat, matched implant-abutment configuration.
Today, the most commonly used implant design is a tapered screw, with a moderately rough implant surface, thus facilitating one-stage surgical procedures and allowing for immediate or early loading protocols. A root-form implant design with a variable-threaded geometry, and a moderately rough surface (NobelActive™, Nobel Biocare, Zurich, Switzerland) has been introduced to allow for immediate placement and anticipated loading protocols. The osteotome effect of the tapered implant body design improves the likelihood of adequate primary stability needed to ensure immediate implant placement and loading. The stress was concentrated around the neck of the implant, and the majority of the stress was distributed around the first six threads of the implant.
Implant Diameter
The choice of implant diameter depends on the volume of the residual bone, the amount of space available for the prosthetic reconstruction, the emergence profile and the type of occlusion. In cases of low bone quality, the optimum increase in the implant length and/or diameter should be taken into account to achieve higher primary stability, measured as implant stability quotient (ISQ).
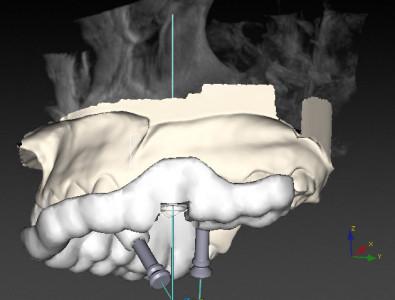
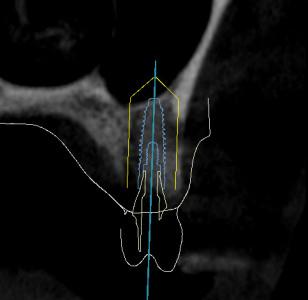
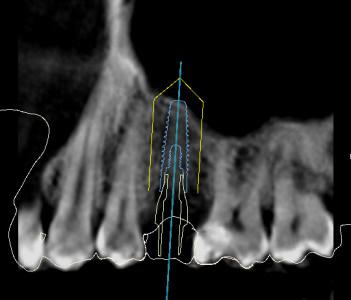
Guided Treatment Planning and Guided Surgery
Guided treatment planning (and guided implant surgery) using cone beam computed tomography (CBCT) in combination with virtual treatment planning software, allows the clinicians to select the ideal implant length and diameter before surgery.
Figure 1 Figure 2 Figure 3 Implant planning using Nobel Clinician software (Nobel Biocare).
Platform Switching
Platform switching is the use of smaller diameter abutments on wider diameter implants. Platform switching implants with a conical implant-abutment connection provide better results in terms of abutment fit, stability, and seal performance, resulting in less horizontal and vertical crestal bone loss, compared to implants restored with a matched implant-abutment design.
Platform switching implants may be of importance in areas of aesthetic concern, reducing the safety distance between the nearest teeth/implants, as well as the risk of an exposed metal implant shoulder.

Figure 4: Platform switching implants; Single crown restorations Intraoral

Figure 5: Platform switching implants; Single crown restorations radiographic view
Figure 6 Figure 7 Figure 8 Platform switched single implant; definitive crown delivery (Figures 6 & 7) and 3 years follow-up (Figure 8).
Smaller Diameter (Narrow) Implants
Narrow-diameter implants have specific clinical indications, for example, they are used in areas where the ridge dimension is narrow and to replace teeth with a small cervical diameter. In the event of missing maxillary lateral incisors and mandibular incisors, where mesiodistal width is often limited (≤6 mm), smaller-diameter implants (<3.5 mm) are recommended to minimize biologic encroachment to the adjacent teeth.

Figure 9: 3.0 NobelActive™ Implant to restore a lower left central incisor.
The implant diameter had a more significant effect than length in terms of relieving the crestal stress and strain concentration. However, decreasing the diameter also means increasing the risk of implant fracture caused by lower mechanical stability and increasing the risk of overload.