-
0
Patient Assessment
- 0.1 Patient Demand
- 0.2 Anatomical location
-
0.3
Patient History
- 2.1 General patient history
- 2.2 Local history
-
0.4
Risk Assessment
- 3.1 Risk Assessment Overview
- 3.2 Age
- 3.3 Patient Compliance
- 3.4 Smoking
- 3.5 Drug Abuse
- 3.6 Recreational Drug and Alcohol Abuse
- 3.7 Condition of Natural Teeth
- 3.8 Parafunctions
- 3.9 Diabetes
- 3.10 Anticoagulants
- 3.11 Osteoporosis
- 3.12 Bisphosphonates
- 3.13 MRONJ
- 3.14 Steroids
- 3.15 Radiotherapy
- 3.16 Risk factors
-
1
Diagnostics
-
2
Treatment Options
-
2.1
Treatment planning
- 0.1 Non-implant based treatment options
- 0.2 Treatment planning conventional, model based, non-guided, semi-guided
- 0.3 Digital treatment planning
- 0.4 NobelClinician and digital workflow
- 0.5 Implant position considerations overview
- 0.6 Soft tissue condition and morphology
- 0.7 Site development, soft tissue management
- 0.8 Hard tissue and bone quality
- 0.9 Site development, hard tissue management
- 0.10 Time to function
- 0.11 Submerged vs non-submerged
- 0.12 Healed or fresh extraction socket
- 0.13 Screw-retained vs. cement-retained
- 0.14 Angulated Screw Channel system (ASC)
- 2.2 Treatment options esthetic zone
- 2.3 Treatment options posterior zone
- 2.4 Comprehensive treatment concepts
-
2.1
Treatment planning
-
3
Treatment Procedures
-
3.1
Treatment procedures general considerations
- 0.1 Anesthesia
- 0.2 peri-operative care
- 0.3 Flap- or flapless
- 0.4 Non-guided protocol
- 0.5 Semi-guided protocol
- 0.6 Guided protocol overview
- 0.7 Guided protocol NobelGuide
- 0.8 Parallel implant placement considerations
- 0.9 Tapered implant placement considerations
- 0.10 3D implant position
- 0.11 Implant insertion torque
- 0.12 Intra-operative complications
- 0.13 Impression procedures, digital impressions, intraoral scanning
- 3.2 Treatment procedures esthetic zone surgical
- 3.3 Treatment procedures esthetic zone prosthetic
- 3.4 Treatment procedures posterior zone surgical
- 3.5 Treatment procedures posterior zone prosthetic
-
3.1
Treatment procedures general considerations
-
4
Aftercare
Abutment and material selection, final restoration, esthetic zone
Key points
- There are a broad range of abutment choices.
- Cement retention requires choosing between custom or prefabricated abutments.
- Screw retention can be achieved by a variety of approaches.
After some period of healing and soft tissue manipulation, the temporary abutment is replaced with a final abutment in preparation for the final restoration. Often, a final abutment can be placed at the time of provisionalization, and therefore the abutment and any attached soft tissue can remain undisturbed at the time of delivery of the final crown.
Abutment Type and Design, Final Restoration
The design of the final abutment is typically decided at the time of treatment planning. Potential options include:
- A “one piece” abutment/restoration (screw retained).
- A custom CAD/CAM abutment can be designed, providing a wider range of emergence profiles and angulation/position correction
- A “stock” abutment can be selected and adapted chair-side or by the dental laboratory
- A UCLA-type castable abutment can be prepared
It is generally accepted that a CAD/CAM abutment provides the ideal overall combination of design flexibility, quality/predictability of manufacture and time-to-delivery. Castable abutments remain common, but can not consistently deliver the same quality as CAD/CAM abutments. Also, the extensive laboratory handling increases the risk of adulteration to the abutment-implant interface (e.g. grit blasting, polishing, nicks).
The abutment can be combined with the final crown and delivered in ‘one piece’ as a screw-retained solution. This has several benefits (see “Screw vs. cement retained” Treatment Guideline).
Chairside preparation of Titanium (or zirconia) stock abutments should be done with the proper burs and copious water irrigation
The positioning of the implant has a significant impact on abutment design. e.g. angulation, position mesial/distal & lingual/palatal. In ideal placement conditions, a screw retained final restoration can be delivered. In many cases of less-than-ideal placement, a screw-retained final restoration can still be an option with either the Angulated Screw Channel (see 3192 - Angulated Screw Channel System (ASC) Treatment Guideline) or a lingual screw.
Abutment Materials, Final Restoration
Material options include titanium, ‘opaqued’ titanium, zirconia (including shaded zirconia), gold-shaded titanium and Gold (UCLA-type abutments).
It is important to minimize the number of times an abutment is removed/replaced – including healing abutments, temporary abutments and permanent abutments, minimizing trauma to the underlying tissue.
The Choice
Following the placement of an endosseous implant the clinician will need to decide on the choice of retention for the final restoration. When there is a choice one will need to choose from the cement or screw retained options. The advantages and disadvantages have been reviewed in other Treatment Guidelines. In clinical presentations where the implant position allows for desirable access to the abutment / prosthetic screw without having to compromise esthetics this is a very desirable approach. This can be achieved even in instances with significant deviation from the long axis by utilizing the angulated screw channel design (ASC), or angulated abutments.
When either the implant position is not desirable or the access to the retaining screw would emerge from the buccal or labial surface a cement approach may be the only option. Therefore implant position will directly affect abutment choice. After adequate healing if a provisional abutment has been used it needs to be replaced by the final abutment. Ideally the choice of the final abutment was decided at the treatment planning stage, NobelClincian software is ideally suited for this. The abutments fall in the following broad categories: Stock, Castable, CAD/CAM, and one piece abutment / restoration. The literature is consistent that CAD/CAM abutments are at least as accurate as cast and prefabricated abutments, with the distinct advantage of having the ability to develop ideal contours to support soft tissue profiles.
Abutment considerations in cement retained implant full crowns
Cementing on an implant abutment can be achieved by either using prefabricated abutments of custom abutments. The prefabricated abutments are available in tooth specific formats that replicate the preparation of a natural tooth. These come in mostly metallic forms and allow for the design of anatomically correct tooth replacements. If one chooses to use a metallic or ceramic abutment and it requires modification this can be achieved intra orally with the use of fine diamonds and copious amounts of water during the preparation procedure.
The custom abutment design allows for the choice of different materials that are either metal, ceramic, or metal connection with ceramic cemented to the them. The choice of which one to use is dependent upon an number of factors including but not limited to: position in the oral cavity, soft tissue profile, adjacent teeth or implants, opposing arch, requirements of material strength, inter arch distance, and the choice of material for the final restoration. The fabrication of these abutments can be accomplished by conventional impression procedures or scanning of the implant position and orientation thru the use of scan bodies.
Abutment considerations in screw retained implant full crowns
The screw retained restoration can be fabricated either as a one piece restoration (abutment / crown all one piece) or separately. In the latter approach the abutment can be placed and the an abutment level impression made, a provisional can be placed to the abutment at that time. . In the one piece final restoration the abutment and final crown may be in various formats: metal ceramic crown, ceramic crown to metal insert that are luted together, or all ceramic. The latter may be problematic in the potential for breakage and wear of the ceramic component that interfaces with the implant connection.
It is also possible to have custom abutments that are then “tapped”, thus using a screw to retain the final restoration to the abutment from a different position. This helps in correcting implant placement issues.
As esthetics is critical and the soft tissue architecture and thickness play a critical role, ceramic abutments will provide a more acceptable esthetic result. The coro-apical position of the implant is also critical to accomplish proper emergence profile. Finally the choice of the abutment must satisfy all aspects of the esthetic needs. The use of various materials such as all ceramic, metals that allow opaquing of the surface or yellow gold will improve the overall esthetic appeal.
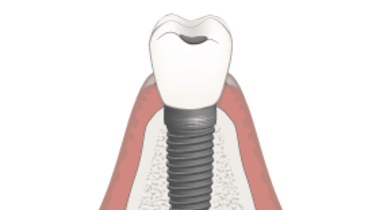
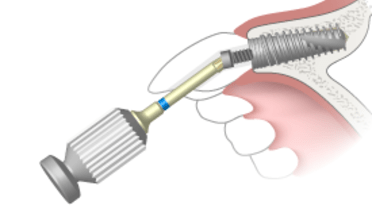
Figure 1 Figure 2
Figures 1 & 2: Ceramic abutments with ceramic substructures

Figure 3: Screw retrained metal ceramic substructure with metal abutments (Not ASC),
one abutment does not allow for screw retention
Figure 4: Lingual tap of metal ceramic custom abutment with full crown