-
0
Patient Assessment
- 0.1 Patient Demand
- 0.2 Anatomical location
-
0.3
Patient History
- 2.1 General patient history
- 2.2 Local history
-
0.4
Risk Assessment
- 3.1 Risk Assessment Overview
- 3.2 Age
- 3.3 Patient Compliance
- 3.4 Smoking
- 3.5 Drug Abuse
- 3.6 Recreational Drug and Alcohol Abuse
- 3.7 Condition of Natural Teeth
- 3.8 Parafunctions
- 3.9 Diabetes
- 3.10 Anticoagulants
- 3.11 Osteoporosis
- 3.12 Bisphosphonates
- 3.13 MRONJ
- 3.14 Steroids
- 3.15 Radiotherapy
- 3.16 Risk factors
-
1
Diagnostics
-
2
Treatment Options
-
2.1
Treatment planning
- 0.1 Non-implant based treatment options
- 0.2 Treatment planning conventional, model based, non-guided, semi-guided
- 0.3 Digital treatment planning
- 0.4 NobelClinician and digital workflow
- 0.5 Implant position considerations overview
- 0.6 Soft tissue condition and morphology
- 0.7 Site development, soft tissue management
- 0.8 Hard tissue and bone quality
- 0.9 Site development, hard tissue management
- 0.10 Time to function
- 0.11 Submerged vs non-submerged
- 0.12 Healed or fresh extraction socket
- 0.13 Screw-retained vs. cement-retained
- 0.14 Angulated Screw Channel system (ASC)
- 2.2 Treatment options esthetic zone
- 2.3 Treatment options posterior zone
- 2.4 Comprehensive treatment concepts
-
2.1
Treatment planning
-
3
Treatment Procedures
-
3.1
Treatment procedures general considerations
- 0.1 Anesthesia
- 0.2 peri-operative care
- 0.3 Flap- or flapless
- 0.4 Non-guided protocol
- 0.5 Semi-guided protocol
- 0.6 Guided protocol overview
- 0.7 Guided protocol NobelGuide
- 0.8 Parallel implant placement considerations
- 0.9 Tapered implant placement considerations
- 0.10 3D implant position
- 0.11 Implant insertion torque
- 0.12 Intra-operative complications
- 0.13 Impression procedures, digital impressions, intraoral scanning
- 3.2 Treatment procedures esthetic zone surgical
- 3.3 Treatment procedures esthetic zone prosthetic
- 3.4 Treatment procedures posterior zone surgical
- 3.5 Treatment procedures posterior zone prosthetic
-
3.1
Treatment procedures general considerations
-
4
Aftercare
Periodontitis
Key points
- Periodontitis affects the majority of the population in various forms.
- Periodontitis can be handled successfully with correct treatment measures in cooperative patients.
- Periodontitis is regarded one risk indicator for peri-implantitis.
Characteristics of periodontal disease
Periodontitis is a most common oral disease and 5 to 20% of any population suffers from its severe forms, while mild and moderate periodontitis affect a majority of adults. Causative factors may be both local and systemic, but regularly one finds plaque-induced inflammations, such as gingivitis and periodontitis, to be the etiological factors. Periodontitis is claimed to result from previous gingivitis, but not all sites with gingivitis will progress to periodontitis. First molars and incisors show normally the first signs of the disease. Patients with periodontitis run a higher risk of developing various systemic diseases, such as heart/vascular diseases and diabetes.
Considerations
A single implant, replacing a missing tooth, will after some time exhibit similar microbial species in the mucosal sulcus/pocket, as found in the gingival sulci/pockets of remaining teeth. Consider the whole jaw situation and condition of all teeth when planning for the replacement of a single missing tooth. It is of outmost importance to gain control of or preferably eliminate any ongoing periodontitis prior to implant placement or a fixed or removable denture. This will require hygiene information/instructions, treatment by an oral hygienist, sometimes periodontal surgery, but above all a dedicated cooperative patient. When treating the periodontitis patient under such circumstances, the outcome is generally predictable and successful.
Figures 1-2: Advanced progression of periodontal disease (arrows) at lower left second bicuspid and lower right second molar. Placing an implant in this environment is not recommended!
Together with smoking, periodontitis is regarded as a possible risk indicator for such patients to develop later peri-implantitis. However, taking into consideration that the overall majority of implant-treated patients show no or few signs of peri-implantitis, and that many of them have had a history of or even have ongoing periodontitis, one is still confused at a clear relationship.
Patient referred for bilateral implants lower jaw. Planned for extractions first left bicuspid, second right bicuspid and bilateral second molars.
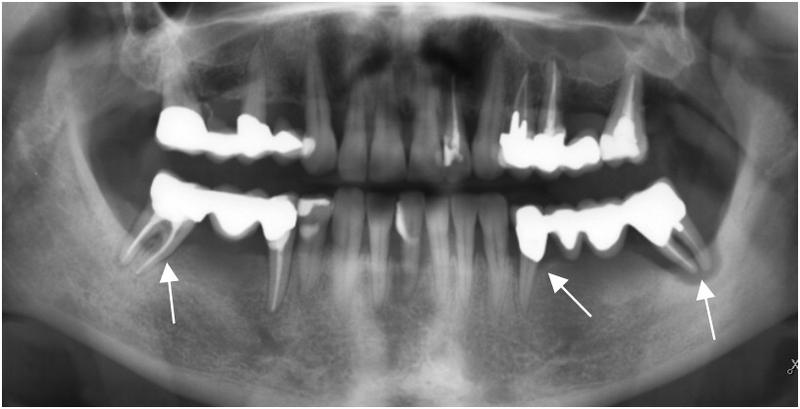
Figure 3: Some teeth exhibiting advanced periodontitis (white arrows).
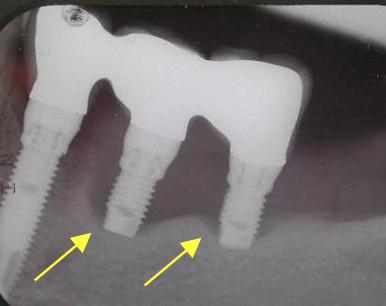
Figures 4 & 5: Three out of five inserted implants developing severe peri-implantitis after 3-4 years (yellow arrows), showing similar site-specific appearance as periodontal disease.

Figure 6: One unaffected single-tooth implant remains on each side after 5 years.