-
0
Patient Assessment
- 0.1 Patient Demand
- 0.2 Anatomical location
-
0.3
Patient History
- 2.1 General patient history
- 2.2 Local history
-
0.4
Risk Assessment
- 3.1 Risk Assessment Overview
- 3.2 Age
- 3.3 Patient Compliance
- 3.4 Smoking
- 3.5 Drug Abuse
- 3.6 Recreational Drug and Alcohol Abuse
- 3.7 Condition of Natural Teeth
- 3.8 Parafunctions
- 3.9 Diabetes
- 3.10 Anticoagulants
- 3.11 Osteoporosis
- 3.12 Bisphosphonates
- 3.13 MRONJ
- 3.14 Steroids
- 3.15 Radiotherapy
- 3.16 Risk factors
-
1
Diagnostics
-
2
Treatment Options
-
2.1
Treatment planning
- 0.1 Non-implant based treatment options
- 0.2 Treatment planning conventional, model based, non-guided, semi-guided
- 0.3 Digital treatment planning
- 0.4 NobelClinician and digital workflow
- 0.5 Implant position considerations overview
- 0.6 Soft tissue condition and morphology
- 0.7 Site development, soft tissue management
- 0.8 Hard tissue and bone quality
- 0.9 Site development, hard tissue management
- 0.10 Time to function
- 0.11 Submerged vs non-submerged
- 0.12 Healed or fresh extraction socket
- 0.13 Screw-retained vs. cement-retained
- 0.14 Angulated Screw Channel system (ASC)
- 2.2 Treatment options esthetic zone
- 2.3 Treatment options posterior zone
- 2.4 Comprehensive treatment concepts
-
2.1
Treatment planning
-
3
Treatment Procedures
-
3.1
Treatment procedures general considerations
- 0.1 Anesthesia
- 0.2 peri-operative care
- 0.3 Flap- or flapless
- 0.4 Non-guided protocol
- 0.5 Semi-guided protocol
- 0.6 Guided protocol overview
- 0.7 Guided protocol NobelGuide
- 0.8 Parallel implant placement considerations
- 0.9 Tapered implant placement considerations
- 0.10 3D implant position
- 0.11 Implant insertion torque
- 0.12 Intra-operative complications
- 0.13 Impression procedures, digital impressions, intraoral scanning
- 3.2 Treatment procedures esthetic zone surgical
- 3.3 Treatment procedures esthetic zone prosthetic
- 3.4 Treatment procedures posterior zone surgical
- 3.5 Treatment procedures posterior zone prosthetic
-
3.1
Treatment procedures general considerations
-
4
Aftercare
MRONJ
Key points
- The terms MRONJ (Medication related osteonecrosis of the jaw) and ARONJ (Antiresorptive drug related osteonecrosis of the jaw) presently replace the term BRONJ.
- MRONJ is similar to osteonecrosis, and is usually identified by the appearance of exposed bone in the oral cavity.
- MRONJ is difficult to treat. If patient is diagnosed with MRONJ, advice and cooperation with entire involved dental and medical rehabilitation team is critical.
- Bisphosphonates (BP) may predispose to ‘bisphosphonate-related osteonecrosis of the jaw’ (BRONJ).
General considerations
A critical side effect in the oro-maxillo-facial region observed in patients undergoing administration over a long period of time and especially intravenously, bisphosphonate therapy may predispose to ‘bisphosphonate-related osteonecrosis of the jaw’ (BRONJ), or 'antiresorptive drug related osteonecrosis of the jaw' (ARONJ). By definition this is an area of exposed bone in the jaw persisting for more than 8 weeks with no history of radiation therapy while having undergone a bisphosphonate or other anti-resorptive drug therapy.
Incidence of ARONJ/MRONJ as a result of bisphosphonate or other anti-resorpive drug treatment of osteoporosis and Paget's disease is between 0.01% - 0.04%. Consequent to bisphosphonate administration for the treatment of bone cancers and metastases, the incidence of BRONJ is 0.8% - 12%.
Medication-related osteonecrosis of the jaw is similar to osteoradionecrosis and very difficult to treat. The affected bone seems to have impaired healing capacity (reduced turnover) and reduced angiogenesis. The result is a reduced capability to deal with infections and trauma (surgery, tooth extractions).
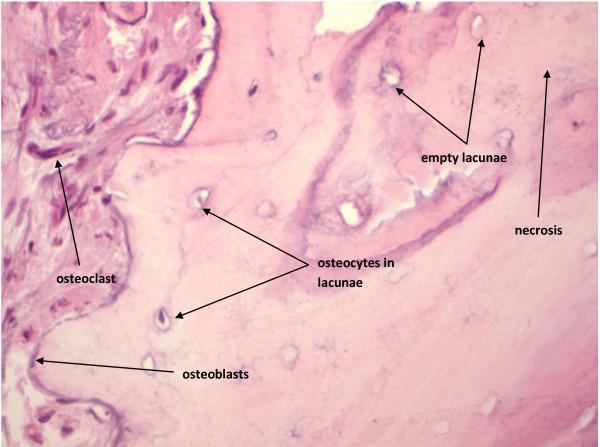
Figure 1: MRONJ - empty lacunae are seen in the center of the bone while towards the surface some lacunae display their osteocytes.
© 2013 Sharma et al.; Vascular Cell 2013 Jan 14;5(1):1. doi: 10.1186/2045-824X-5-1.
MRONJ treatment considerations
If patient is diagnosed with MRONJ, surgery and tooth extraction should be avoided. Hygiene measures should be reassessed and reinforced. This conditions requires a team approach and regular communication between GP, internist, dentist and oral and maxillofacial surgeon.
Detailed and extensive clinical practice guidelines for management of the bisphosphonate patient are available. Some fundamental treatment steps to be used are:
- Daily irrigation and antimicrobial rinse
- Antibiotics to control infection
- Surgical treatment to remove the necrotic bone may be advisable in more advanced cases
- In some patients a removable appliance to cover and protect the exposed bone is necessary
- Protective stent damages the surrounding soft tissues or makes normal function difficult
- If dentures are worn, minimize irritation of the soft-tissues, particularly for patients who are receiving IV bisphosphonate therapy. Dentures should be removed and thoroughly cleaned at night.
(Content © Copyright AAOMS 2008-2013)
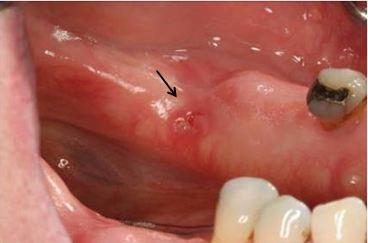
Figure 2: Clinical image of BRONJ.
Courtesy of Dr. Sreenivas Koka, San Diego


MRONJ Treatment
Being diagnosed with MRONJ recently I'm wanting to know how I can treat this condition.
Presently I'm using Curasept gel, Curasept mouthwash & Aloevera plant (for bleeding).
Is there anything else I should or could do.what do you suggest for pain.
Hoping you can give me some advise, ease. I have had the condition approx 5 months.
With kind regards
Lorraine
HARDWICKE BAY
SOUTH AUSTRALIA
AUSTRALIA
Being diagnosed with MRONJ recently I'm wanting to know how I can treat this condition.
Presently I'm using Curasept gel, Curasept mouthwash & Aloevera plant (for bleeding).
Is there anything else I should or could do.what do you suggest for pain.
Hoping you can give me some advise, ease. I have had the condition approx 5 months.
With kind regards
Lorraine
HARDWICKE BAY
SOUTH AUSTRALIA
AUSTRALIA