-
0
Patient Assessment
- 0.1 Patient Demand
- 0.2 Anatomical location
-
0.3
Patient History
- 2.1 General patient history
- 2.2 Local history
-
0.4
Risk Assessment
- 3.1 Risk Assessment Overview
- 3.2 Age
- 3.3 Patient Compliance
- 3.4 Smoking
- 3.5 Drug Abuse
- 3.6 Recreational Drug and Alcohol Abuse
- 3.7 Condition of Natural Teeth
- 3.8 Parafunctions
- 3.9 Diabetes
- 3.10 Anticoagulants
- 3.11 Osteoporosis
- 3.12 Bisphosphonates
- 3.13 MRONJ
- 3.14 Steroids
- 3.15 Radiotherapy
- 3.16 Risk factors
-
1
Diagnostics
-
2
Treatment Options
-
2.1
Treatment planning
- 0.1 Non-implant based treatment options
- 0.2 Treatment planning conventional, model based, non-guided, semi-guided
- 0.3 Digital treatment planning
- 0.4 NobelClinician and digital workflow
- 0.5 Implant position considerations overview
- 0.6 Soft tissue condition and morphology
- 0.7 Site development, soft tissue management
- 0.8 Hard tissue and bone quality
- 0.9 Site development, hard tissue management
- 0.10 Time to function
- 0.11 Submerged vs non-submerged
- 0.12 Healed or fresh extraction socket
- 0.13 Screw-retained vs. cement-retained
- 0.14 Angulated Screw Channel system (ASC)
- 2.2 Treatment options esthetic zone
- 2.3 Treatment options posterior zone
- 2.4 Comprehensive treatment concepts
-
2.1
Treatment planning
-
3
Treatment Procedures
-
3.1
Treatment procedures general considerations
- 0.1 Anesthesia
- 0.2 peri-operative care
- 0.3 Flap- or flapless
- 0.4 Non-guided protocol
- 0.5 Semi-guided protocol
- 0.6 Guided protocol overview
- 0.7 Guided protocol NobelGuide
- 0.8 Parallel implant placement considerations
- 0.9 Tapered implant placement considerations
- 0.10 3D implant position
- 0.11 Implant insertion torque
- 0.12 Intra-operative complications
- 0.13 Impression procedures, digital impressions, intraoral scanning
- 3.2 Treatment procedures esthetic zone surgical
- 3.3 Treatment procedures esthetic zone prosthetic
- 3.4 Treatment procedures posterior zone surgical
- 3.5 Treatment procedures posterior zone prosthetic
-
3.1
Treatment procedures general considerations
-
4
Aftercare
Time to function
Key points
- Main considerations of 'time to function' are immediate, early and conventional time frames for restored function.
- When specific criteria and protocols are met, immediate function is regarded as providing a safe and predictable treatment outcome.
- Immediate function may logically reduce overall treatment time.
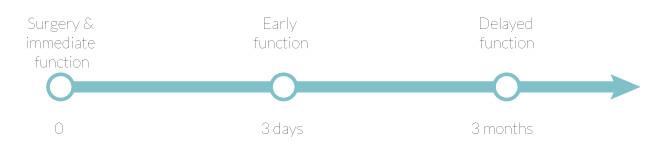
Figure 1: Time to function - options.
Conventional (Delayed) Function
Traditional endosseous oral implant treatment protocols ad modum Brånemark required a variable healing period (usually 3-6 months) before single-crown placement. The healing period was considered necessary to achieve osseointegration and establish a load-bearing interface. The traditional protocol is referred to as “conventional function” and has yielded very good long-term clinical results.
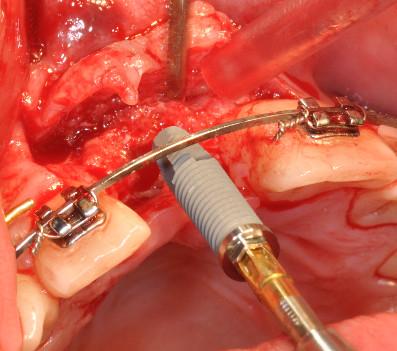
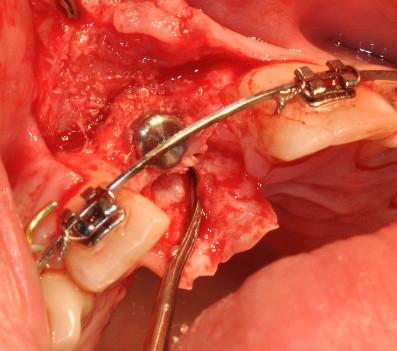
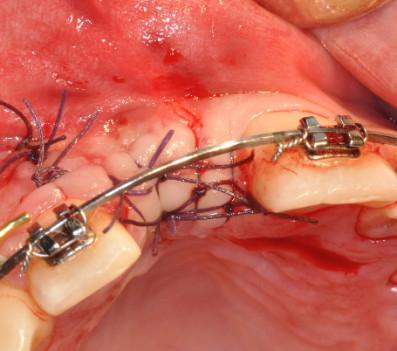
Figures 2: Placement of implant in upper right central incisor region according to the “conventional function” concept.
Figures 3: Placement of implant in upper left lateral incisor region according to the “delayed function” concept.
Early Function
“Early function” refers to single-crown placement from 3 days to 3 months after implant placement. Compared to immediate and conventional function protocols, it has led to comparable documented clinical outcomes.
Immediate Function
The single-crown loading protocol change to one occurring within 3 days of implant placement is referred to as “immediate function”. It has led to promising documented clinical outcomes when judged in the context differences in bone loss, single-crown or implant failure, when compared to “delayed function” documentation. Advantages for the patient include reduction in time from implant placement to restored function and an overall reduction in treatment time.
Current experience indicates that oral implants with good primary stability are candidates for immediate function. Primary stability is popularly ascertained either through the surgeon’s feel or through a surrogate measure of stability (insertion torque or resonance frequency analysis RFA). In the absence of good primary implant stability an immediate function protocol is contraindicated.
While immediate function can be considered in many treatment scenarios, the probability of success is high for the single-tooth situation with adjacent teeth present to take the major load, and the provisional crown adjusted to non-functional load.
Figures 4: Placement of implant in lower right central incisor region according to the “immediate function” concept.