-
0
Patient Assessment
- 0.1 Patient Demand
- 0.2 Anatomical location
-
0.3
Patient History
- 2.1 General patient history
- 2.2 Local history
-
0.4
Risk Assessment
- 3.1 Risk Assessment Overview
- 3.2 Age
- 3.3 Patient Compliance
- 3.4 Smoking
- 3.5 Drug Abuse
- 3.6 Recreational Drug and Alcohol Abuse
- 3.7 Condition of Natural Teeth
- 3.8 Parafunctions
- 3.9 Diabetes
- 3.10 Anticoagulants
- 3.11 Osteoporosis
- 3.12 Bisphosphonates
- 3.13 MRONJ
- 3.14 Steroids
- 3.15 Radiotherapy
- 3.16 Risk factors
-
1
Diagnostics
-
2
Treatment Options
-
2.1
Treatment planning
- 0.1 Non-implant based treatment options
- 0.2 Treatment planning conventional, model based, non-guided, semi-guided
- 0.3 Digital treatment planning
- 0.4 NobelClinician and digital workflow
- 0.5 Implant position considerations overview
- 0.6 Soft tissue condition and morphology
- 0.7 Site development, soft tissue management
- 0.8 Hard tissue and bone quality
- 0.9 Site development, hard tissue management
- 0.10 Time to function
- 0.11 Submerged vs non-submerged
- 0.12 Healed or fresh extraction socket
- 0.13 Screw-retained vs. cement-retained
- 0.14 Angulated Screw Channel system (ASC)
- 2.2 Treatment options esthetic zone
- 2.3 Treatment options posterior zone
- 2.4 Comprehensive treatment concepts
-
2.1
Treatment planning
-
3
Treatment Procedures
-
3.1
Treatment procedures general considerations
- 0.1 Anesthesia
- 0.2 peri-operative care
- 0.3 Flap- or flapless
- 0.4 Non-guided protocol
- 0.5 Semi-guided protocol
- 0.6 Guided protocol overview
- 0.7 Guided protocol NobelGuide
- 0.8 Parallel implant placement considerations
- 0.9 Tapered implant placement considerations
- 0.10 3D implant position
- 0.11 Implant insertion torque
- 0.12 Intra-operative complications
- 0.13 Impression procedures, digital impressions, intraoral scanning
- 3.2 Treatment procedures esthetic zone surgical
- 3.3 Treatment procedures esthetic zone prosthetic
- 3.4 Treatment procedures posterior zone surgical
- 3.5 Treatment procedures posterior zone prosthetic
-
3.1
Treatment procedures general considerations
-
4
Aftercare
Hard tissue and bone quality
Key points
- Jaw bone quality is difficult to define. It is merely described in quantitative measures.
- Bone quality/bone hardness should preferably be identified for each individual implant site and not as one given value for the entire jaw.
- Change of jaw bone quality may be load- and/or age-related.
Bone quality definition
A clear definition of bone quality does not exist. It has been related to mechanical properties of the bone, such as elastic modulus, strength, stiffness, micro-damage, strain, the ability to adapt to specific loads, and the capability to remodel. A more practical suggestion could be to rate the bone hardness experienced during drilling of implant sites. Such a subjective measure would be dependent on the state of mineralization, the coarseness and contiguity of the trabecular bone and the width of cortical layers and thus correlated to the experience of the performing surgeon.
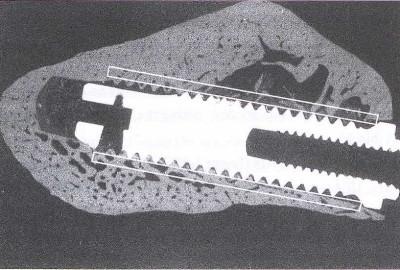
Fig 1: Microradiograph of an implant in mandibular bone. Corridors along the implant periphery denote bone quality regions of interest during implant placement
Measurement techniques
Various techniques have been described for jaw bone quality measurements using conventional radiographs, quantitative computed tomography (expressed in Hounsfield units), bone mineral density (BMD) measurements, jaw bone biopsies, true cutting resistance, etc. However, all these techniques mainly express the bone characteristics in quantity measures, either by rating the bone structures obtained from radiographs and histomorphometry, or by analyzing the bone mineral content.
A proposed and most used jaw bone classification based on preoperative radiographs rated the quality from 1 to 4, depending on the amount of compact and cancellous bone present. The index is however blunt and only suggested to provide one value for the entire jaw.
The true cutting resistance constitutes the major part of the insertion torque together with friction and the contribution of bone sliver packing in deeper preparations. It is defined as “the energy needed to cut out a specific amount of bone material with a tool”, as based on the consumed electric current during low speed drilling. It is thus possible to obtain an objective value, expressing the bone quality in terms of bone hardness in each individual implant site.
Inner bone dimensions
Increased trabecular bone density is frequently seen in anterior compared to posterior jaw regions of both maxillae and mandibles. Thicker cortices are reported in the anterior maxillae while in the tuberosity region fatty marrow and only small clusters of bone dominate. Loss of teeth and thus loss of chewing ability may alter the bone texture. Cortical bone tends to show increased porosity with age, which may be in line with development of post-menopausal osteoporosis in females and senile osteoporosis in both genders. Implant treatment causes load-related bone formation, which could minimize, or even counteract, the physiologic age-related loss of bone mineral content seen in osteoporosis.
