-
0
Patient Assessment
- 0.1 Patient Demand
- 0.2 Anatomical location
-
0.3
Patient History
- 2.1 General patient history
- 2.2 Local history
-
0.4
Risk Assessment
- 3.1 Risk Assessment Overview
- 3.2 Age
- 3.3 Patient Compliance
- 3.4 Smoking
- 3.5 Drug Abuse
- 3.6 Recreational Drug and Alcohol Abuse
- 3.7 Condition of Natural Teeth
- 3.8 Parafunctions
- 3.9 Diabetes
- 3.10 Anticoagulants
- 3.11 Osteoporosis
- 3.12 Bisphosphonates
- 3.13 MRONJ
- 3.14 Steroids
- 3.15 Radiotherapy
- 3.16 Risk factors
-
1
Diagnostics
-
2
Treatment Options
-
2.1
Treatment planning
- 0.1 Non-implant based treatment options
- 0.2 Treatment planning conventional, model based, non-guided, semi-guided
- 0.3 Digital treatment planning
- 0.4 NobelClinician and digital workflow
- 0.5 Implant position considerations overview
- 0.6 Soft tissue condition and morphology
- 0.7 Site development, soft tissue management
- 0.8 Hard tissue and bone quality
- 0.9 Site development, hard tissue management
- 0.10 Time to function
- 0.11 Submerged vs non-submerged
- 0.12 Healed or fresh extraction socket
- 0.13 Screw-retained vs. cement-retained
- 0.14 Angulated Screw Channel system (ASC)
- 2.2 Treatment options esthetic zone
- 2.3 Treatment options posterior zone
- 2.4 Comprehensive treatment concepts
-
2.1
Treatment planning
-
3
Treatment Procedures
-
3.1
Treatment procedures general considerations
- 0.1 Anesthesia
- 0.2 peri-operative care
- 0.3 Flap- or flapless
- 0.4 Non-guided protocol
- 0.5 Semi-guided protocol
- 0.6 Guided protocol overview
- 0.7 Guided protocol NobelGuide
- 0.8 Parallel implant placement considerations
- 0.9 Tapered implant placement considerations
- 0.10 3D implant position
- 0.11 Implant insertion torque
- 0.12 Intra-operative complications
- 0.13 Impression procedures, digital impressions, intraoral scanning
- 3.2 Treatment procedures esthetic zone surgical
- 3.3 Treatment procedures esthetic zone prosthetic
- 3.4 Treatment procedures posterior zone surgical
- 3.5 Treatment procedures posterior zone prosthetic
-
3.1
Treatment procedures general considerations
-
4
Aftercare
Radiographic control
Key points
- Cross-sectional imaging are only justified in the presence of certain symptoms, except as part of ethically approved clinical research and informed consent based on the Helsinki Declaration. Anamnesis and/or clinical examination which indicate demand for further examination.
- In cases of post-operative complications, conventional radiographs might provide additional information. In case of postoperative infections in relation to sinus cavities close to implants, or suspected nerve damage, cross-sectional imaging may be justified.
- Digital radiographs are superior, since allowing a low radiation dose for the patient.
Type of radiographs chosen
Clinicians who provide diagnostic imaging services should always consider the optimum imaging technique for the patient/procedure, even if this means referral to another center.
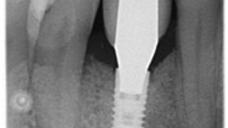
Digital intraoral radiography taken with the paralleling technique are the best way to monitor on-going health around a dental implant, to measure the marginal bone level, to check the proper abutment-to-implant adaptation and the potential presence of subgingival cement*. A baseline image should always be taken once an implant is restored so that there is a way to determine if there is bone loss over time, after the initial, physiological, bone resorption. Nevertheless, a relationship between probing and radiographic evaluation may be used to assess examination needs, suggesting that when changes in probing levels occur, radiographic assessment may be advised.
Radiographs once a year around an implant is the best time to follow-up the peri-implant bone health. Implant threads allow precise distance calculations with the shoulder or the top of the implant as reference point. Generally, bone loss of >1 mm within the first year of implant placement and >0.1 mm annually, may indicate a problem.
Intraoral radiographs are superior to panoramic radiography. The clinicians should be aware of distortions and magnification inherent to panoramic imaging because of projection geometry. Furthermore, parallelism of implants cannot be checked on panoramic radiography.
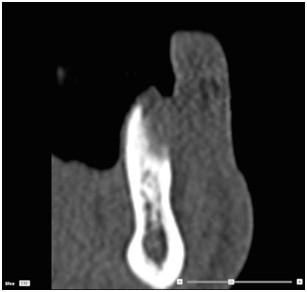
Cone beam computer tomography (CBCT) scan may be the method of choice if case of doubts of in case of post-operative major complications. CBCT scan also allows for evaluating bone augmentation procedures in the oral cavity (guided bone regeneration) or in the maxillary sinus.
Figure 1: Pre-clinical situation Figure 2: CT scan after tooth extraction Figure 3: Surgical view
Figure 4: CT scan at the II stage Figure 5: 1-year intraoral view Figure 6: 1-year radiograph
* Not all cements are visible in radiographs