-
0
Patient Assessment
- 0.1 Patient Demand
- 0.2 Anatomical location
-
0.3
Patient History
- 2.1 General patient history
- 2.2 Local history
-
0.4
Risk Assessment
- 3.1 Risk Assessment Overview
- 3.2 Age
- 3.3 Patient Compliance
- 3.4 Smoking
- 3.5 Drug Abuse
- 3.6 Recreational Drug and Alcohol Abuse
- 3.7 Condition of Natural Teeth
- 3.8 Parafunctions
- 3.9 Diabetes
- 3.10 Anticoagulants
- 3.11 Osteoporosis
- 3.12 Bisphosphonates
- 3.13 MRONJ
- 3.14 Steroids
- 3.15 Radiotherapy
- 3.16 Risk factors
-
1
Diagnostics
-
2
Treatment Options
-
2.1
Treatment planning
- 0.1 Non-implant based treatment options
- 0.2 Treatment planning conventional, model based, non-guided, semi-guided
- 0.3 Digital treatment planning
- 0.4 NobelClinician and digital workflow
- 0.5 Implant position considerations overview
- 0.6 Soft tissue condition and morphology
- 0.7 Site development, soft tissue management
- 0.8 Hard tissue and bone quality
- 0.9 Site development, hard tissue management
- 0.10 Time to function
- 0.11 Submerged vs non-submerged
- 0.12 Healed or fresh extraction socket
- 0.13 Screw-retained vs. cement-retained
- 0.14 Angulated Screw Channel system (ASC)
- 2.2 Treatment options esthetic zone
- 2.3 Treatment options posterior zone
- 2.4 Comprehensive treatment concepts
-
2.1
Treatment planning
-
3
Treatment Procedures
-
3.1
Treatment procedures general considerations
- 0.1 Anesthesia
- 0.2 peri-operative care
- 0.3 Flap- or flapless
- 0.4 Non-guided protocol
- 0.5 Semi-guided protocol
- 0.6 Guided protocol overview
- 0.7 Guided protocol NobelGuide
- 0.8 Parallel implant placement considerations
- 0.9 Tapered implant placement considerations
- 0.10 3D implant position
- 0.11 Implant insertion torque
- 0.12 Intra-operative complications
- 0.13 Impression procedures, digital impressions, intraoral scanning
- 3.2 Treatment procedures esthetic zone surgical
- 3.3 Treatment procedures esthetic zone prosthetic
- 3.4 Treatment procedures posterior zone surgical
- 3.5 Treatment procedures posterior zone prosthetic
-
3.1
Treatment procedures general considerations
-
4
Aftercare
Implant position esthetic zone
Key points
- Implant placement in the anterior region is one of the most challenging surgical procedures in terms of esthetic outcome and patient’s awareness of this sensitive region.
- Careful clinical evaluation prior to implant surgery in terms of hard and soft tissue.
- Implant supported single crowns have the highest estimated 10-year survival rate (89.4%) compared to conventional FDP (89.2%), cantilever FDP (80.3%), implant-supported FDP (86.7%), combined tooth-implant-supported FDP (77.8%) and resin-bonded bridges (65%) (Pjetursson et al. 2008).
- Alternatives: removable partial denture (RPD), three-unit fixed prosthesis, resin-bonded bridge (Maryland), cantilevered prosthesis.
Anatomical considerations
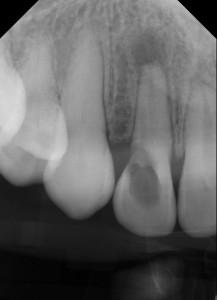
Prior to implant placement a thorough radiographic (e.g. conventional/panoramic x-ray, CT scan, cone beam CT) and clinical evaluation (Angle's class, adjacent teeth, gingival biotype, recessions, mesiodistal width) is indicated. Anatomic landmarks of particular interest in the anterior maxillary region are the nasopalatine (incisive) canal/nerve, the nasal floor, an extremely extended maxillary sinus into the canine region, descending branches of the infraorbital nerve and apical root convergence/root proximity of adjacent teeth (Greenstein, Cavallaro, and Tarnow 2008).
The ideal implant position in the esthetic zone
The following points should be assured in order to rehabilitate a tooth gap in the anterior region with an implant: at least 6mm gap width in mesiodistal extension to allow a distance of 1.5mm or more from adjacent teeth, at least 6 mm buccolingual bone volume to allow 1.5mm or more on the facial/buccal site and a minimum of 0.5mm on the palatal site.
Shorter implants (<10mm) may be indicated if there is an insufficient bone height. Maintenance of at least 1.5mm distance to adjacent teeth should avoid the resorption of interproximal bone. If resorption in the interproximal area occurs, papilla formation can be impaired as the distance between bone and contact point should not exceed 5mm (Tarnow, Magner, and Fletcher 1992).
The angulation of the implant axis partly determines the facial emergence profile of the final crown. The implant body should be positioned according to the facial position of the crown of the adjacent teeth, directly under the incisal edge or under the cingulum. The latter often allows screw-retained crowns as the screw access hole is situated within the cingulum. Too facial positioning may result in the use of cement-retained crowns or angled abutment screws. The best esthetic outcome is accomplished by positioning the implant body under the incisal edge.
Another important factor, which influences the emergence profile, is the depth of the implant body. Shallow positioning of less than 2mm below the free gingival margin (FGM) could lead to visible parts of the titanium screw. Deep positioning of more than 4mm below the cementoenamel junction could result in greater probing depths, which is possibly linked to bone loss. The ideal depth is situated between 2 and 4mm below the FGM of the adjacent teeth (Nisapakultorn et al. 2010).
In order to gain a sufficient amount of bone on the facial site (at least 1.5mm or more) and to direct the implant axis through the incisal edge of the final crown a slightly palatal positioning of the implant is necessary.
Implant insertion depth, palatal wall, bucall plate, gap considerations, mesio distal distance to adjacent teeth .
Figure 1: Initial situation: perforation of the crown and chronic apical periodontitis on tooth #12 (#7 UNIV) Figure 2: Provisional restoration (resin-bonded) after extraction of tooth #12 (#7 UNIV) Figure 3: Clinical situation before implant placement

Figure 4: Postoperative radiograph after implant placement
Figure 5: Immediate provisional restoration after implant placement Figure 6: Clinical situation 2 weeks after implant placement Figure 7: Clinical situation 3 months after implant placement