-
0
Patient Assessment
- 0.1 Patient Demand
- 0.2 Anatomical location
-
0.3
Patient History
- 2.1 General patient history
- 2.2 Local history
-
0.4
Risk Assessment
- 3.1 Risk Assessment Overview
- 3.2 Age
- 3.3 Patient Compliance
- 3.4 Smoking
- 3.5 Drug Abuse
- 3.6 Recreational Drug and Alcohol Abuse
- 3.7 Condition of Natural Teeth
- 3.8 Parafunctions
- 3.9 Diabetes
- 3.10 Anticoagulants
- 3.11 Osteoporosis
- 3.12 Bisphosphonates
- 3.13 MRONJ
- 3.14 Steroids
- 3.15 Radiotherapy
- 3.16 Risk factors
-
1
Diagnostics
-
2
Treatment Options
-
2.1
Treatment planning
- 0.1 Non-implant based treatment options
- 0.2 Treatment planning conventional, model based, non-guided, semi-guided
- 0.3 Digital treatment planning
- 0.4 NobelClinician and digital workflow
- 0.5 Implant position considerations overview
- 0.6 Soft tissue condition and morphology
- 0.7 Site development, soft tissue management
- 0.8 Hard tissue and bone quality
- 0.9 Site development, hard tissue management
- 0.10 Time to function
- 0.11 Submerged vs non-submerged
- 0.12 Healed or fresh extraction socket
- 0.13 Screw-retained vs. cement-retained
- 0.14 Angulated Screw Channel system (ASC)
- 2.2 Treatment options esthetic zone
- 2.3 Treatment options posterior zone
- 2.4 Comprehensive treatment concepts
-
2.1
Treatment planning
-
3
Treatment Procedures
-
3.1
Treatment procedures general considerations
- 0.1 Anesthesia
- 0.2 peri-operative care
- 0.3 Flap- or flapless
- 0.4 Non-guided protocol
- 0.5 Semi-guided protocol
- 0.6 Guided protocol overview
- 0.7 Guided protocol NobelGuide
- 0.8 Parallel implant placement considerations
- 0.9 Tapered implant placement considerations
- 0.10 3D implant position
- 0.11 Implant insertion torque
- 0.12 Intra-operative complications
- 0.13 Impression procedures, digital impressions, intraoral scanning
- 3.2 Treatment procedures esthetic zone surgical
- 3.3 Treatment procedures esthetic zone prosthetic
- 3.4 Treatment procedures posterior zone surgical
- 3.5 Treatment procedures posterior zone prosthetic
-
3.1
Treatment procedures general considerations
-
4
Aftercare
Non-guided protocol
Key points
- Non-guided = “free-hand” approach.
- Experienced skills in implant dentistry.
- Profound knowledge of oral anatomy.
- Radiologic evaluation of implant site (panoramic x-ray and/or CT scan).
- Reduced costs for the patient.
Clinician Experience
The experienced surgeon may place implants non guided, i.e. in a “free-hand” approach. Especially in the early phase of the learning curve it may be advantageous not to force this approach as a guided-approach facilitates correct implant positions.
However, the free-hand approach is subjected to “easy” cases with sufficient amount of bone.
In cases of implant placement without a CT or CBCT scan, insufficient amount of bone may present after surgical incision and elevation of a mucoperiosteal flap. Additional costs would arise for the patient as simultaneous augmentation and implant placement or a 2-stage approach is indicated.
Limitations
Limitations of this approach are that incorrect positioning of the implant may drive it useless for prosthetic rehabilitation – in severe cases even with angled abutments, damage to adjacent teeth, damage to neurovascular structures and loss of primary stability due to multiple correction of the position (after the first drill). In order to avoid the latter it is advisable to not prepare until the full length of the implant with the first drill and instead to check the axis (three-dimensional) after 6 mm (or even less).
Cost
Conventional free-hand implant placement reduces the costs for the patient, as a CT scan with consecutive virtual planning and printing of a surgical template are not required.
Accuracy
Studies have compared the accuracy between guided and conventional implant surgery and found significant differences in favor of guided protocols (Nickenig et al. 2010; Kramer et al. 2005; Hoffmann et al. 2005). As non-guided implant placement necessitates more experience, its use will be restricted to the experienced surgeon and “easy” cases. However, a panoramic x-ray and/or CT scan is important to allow identification of bone height and anatomic landmarks. Bone width may only be estimated by clinical palpation and intraoral measuring (in case of no available CT scan), which is strongly influenced by tissue width and may render false positive values of bone width.
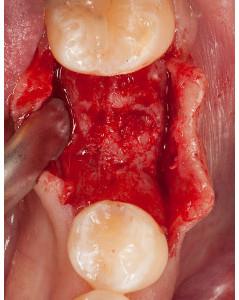
Figure 1: Intermediate gap region #36 (#19 UNIV) Figure 2: Clinical situation after raising a mucoperiosteal flap Figure 3: Control of implant position: the direction indicator points to mesiopalatal cusp of the first upper molar
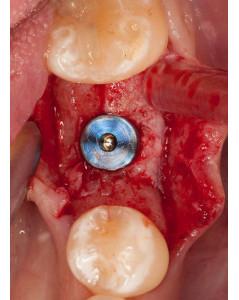
F igure4: Implant bed preparation Figure 5: Inserted implant in region #36 (19 UNIV) Figure 6: Wound closure with single and criss-cross sutures