-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
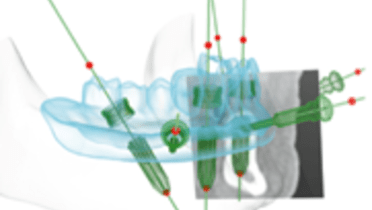
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
Imaging tools overview
Key points
- There is a legal and ethical need to weigh the risks and benefits of imaging and radiation exposure
- It is better to refer the patient rather than perform procedures that provide incomplete imaging information
- For many implant surgeries, 3D imaging provides valuable information to assist in diagnosis and treatment planning
Main imaging tools
Because any form or radiation can impose a risk, patient history and clinical examination should be performed first to ensure that the right kind of imaging is sought and unhelpful imaging is avoided.
The four main types of imaging tools utilized, and discussed in greater detail in other sections are:
- Intra-oral radiographs
- Panoramic radiographs
- Spiral CT
- Cone beam CT (CBCT)
Radiological μSv (Microsievert) dosages:
Intra-oral radiograph
1
Panoramic radiograph 4-30
4-30
Lateral cephalogram
7-10
Spiral CT maxilla 100-3300
100-3300
Spiral CT mandible
400-1200
Spiral CT skull
2000
CBCT large field of view 70-1000
70-1000
CBCT small field of view
50-650
Chest radiograph
50
Natural annual radiation (regional variations!)
~ 2500
Clinical topics
Related articles
Additional resources
Additional external resources
Questions
Ask a question
Log in or sign up to continue
You have reached the limit of content accessible without log in or this content requires log in. Log in or sign up now to get unlimited access to all FOR online resources.
No payments necessary - FOR is completely free of charge.