-
0
Patient Assessment
- 0.1 Patient Demand
- 0.2 Anatomical location
-
0.3
Patient History
- 2.1 General patient history
- 2.2 Local history
-
0.4
Risk Assessment
- 3.1 Risk Assessment Overview
- 3.2 Age
- 3.3 Patient Compliance
- 3.4 Smoking
- 3.5 Drug Abuse
- 3.6 Recreational Drug and Alcohol Abuse
- 3.7 Condition of Natural Teeth
- 3.8 Parafunctions
- 3.9 Diabetes
- 3.10 Anticoagulants
- 3.11 Osteoporosis
- 3.12 Bisphosphonates
- 3.13 MRONJ
- 3.14 Steroids
- 3.15 Radiotherapy
- 3.16 Risk factors
-
1
Diagnostics
-
2
Treatment Options
-
2.1
Treatment planning
- 0.1 Non-implant based treatment options
- 0.2 Treatment planning conventional, model based, non-guided, semi-guided
- 0.3 Digital treatment planning
- 0.4 NobelClinician and digital workflow
- 0.5 Implant position considerations overview
- 0.6 Soft tissue condition and morphology
- 0.7 Site development, soft tissue management
- 0.8 Hard tissue and bone quality
- 0.9 Site development, hard tissue management
- 0.10 Time to function
- 0.11 Submerged vs non-submerged
- 0.12 Healed or fresh extraction socket
- 0.13 Screw-retained vs. cement-retained
- 0.14 Angulated Screw Channel system (ASC)
- 2.2 Treatment options esthetic zone
- 2.3 Treatment options posterior zone
- 2.4 Comprehensive treatment concepts
-
2.1
Treatment planning
-
3
Treatment Procedures
-
3.1
Treatment procedures general considerations
- 0.1 Anesthesia
- 0.2 peri-operative care
- 0.3 Flap- or flapless
- 0.4 Non-guided protocol
- 0.5 Semi-guided protocol
- 0.6 Guided protocol overview
- 0.7 Guided protocol NobelGuide
- 0.8 Parallel implant placement considerations
- 0.9 Tapered implant placement considerations
- 0.10 3D implant position
- 0.11 Implant insertion torque
- 0.12 Intra-operative complications
- 0.13 Impression procedures, digital impressions, intraoral scanning
- 3.2 Treatment procedures esthetic zone surgical
- 3.3 Treatment procedures esthetic zone prosthetic
- 3.4 Treatment procedures posterior zone surgical
- 3.5 Treatment procedures posterior zone prosthetic
-
3.1
Treatment procedures general considerations
-
4
Aftercare
Semi-guided protocol
Key points
- Accurate implant placement can be performed in a template assisted, fully- or semi-guided procedure.
- Treatment plans can easily be shared with collaborators or referring clinicians.
- Regular calibration procedure ensure accurate imaging segmentation of the radiographic guide.
Today it is widely accepted that implant surgery benefits from computer-guided template-assisted surgery, particularly in complex situations. It is well understood that an accurate implant planning is critical to achieve an optimal prosthetic result.
In addition to the traditional fully guided approach, NobelClinician software offers the possibility to choose a “semi guided approach”, using only the initial guided pilot drill. The clinician is always freedom to decide between freehand, fully guided or pilot guided surgery during the course of planning, offering great flexibility in treatment management.
The surgical guide for use in implant treatment is fabricated based on the patient’s anatomy and the planned implant positions. Tridimensional orientation and depth of the first drill are crucial steps during the implant site preparation. The NobelGuide pilot drill template helps to overcome this challenge by setting the preplanned drilling trajectory and depth while still enabling clinicians to finish the surgery using freehand techniques. This approach is very helpful in single implants due to the reduced diameter of the sleeve that allows it to be positioned between two adjacent teeth. An optional wax-up can be added into the planning process to help the clinician plan the best possible implant position based on the prosthetic requirements.
Studies evaluating the cost efficiency and treatment time of different treatment work flows are scarce. However, clinicians should inform patients that computer-assisted template-based surgery implies an increased planning time and slightly additional costs. However, the additional cost should be analyzed in terms of cost-effectiveness and consider the reduction of surgery time and post-operative pain and swelling, as well as, the possible increased accuracy. In fact, digital workflow has been shown to be more efficient than the conventional pathway, reducing the overall treatment time and costs. Avoidance of critical anatomic structures, the aesthetic and functional advantages of prosthodontic-driven implant positioning must also be considered.
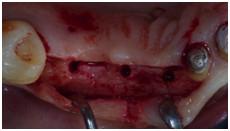
Figure 1 Figure 2 Figure 3
Figures 1-3: Implant placement using semi guided protocol. Pilot guided drill (Figure 1); flap elevation (Figure 2); peri-apical radiographs showing one-stage approach and trascrestal sinus floor elevation (Figure 3).