-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
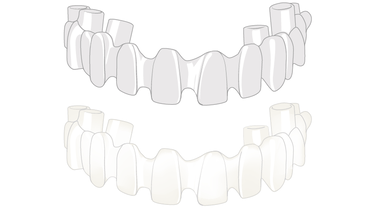
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
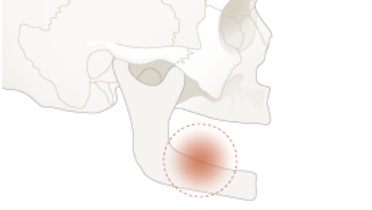
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
Cement-retained restorations, overview
Key points
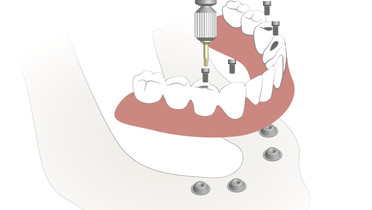
- Cement-retained restorations are a traditional design option allowing for passive fit
- Offers advantages especially in the esthetic zone, as abutment screw channel opening does not affect esthetic bridge design
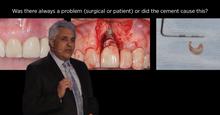
- Subgingival cement is a main reason for peri-implant tissue inflammation, meticulous removal of cement excess is crucial for peri-implant tissue health
- Today, CAD/CAM scanning and milling of the restoration provides high precision and passive fit
- To avoid potential complications related to cementation procedures, especially in edentulous situations a screw-retained CAD/CAM fabricated construction is nowadays the option of choice
Indication and principle considerations
Cement-retained restorations are a traditional design to attach a restoration (crown, bridge) to an implant-retained abutment, similar to cementing a crown or bridge restoration on a natural tooth. With the traditional, relatively imprecise cast techniques, the cement-retained design was one of the technicalities to obtain the necessary passive fit of long-span multi-unit restorations over the implants. CAD/CAM scanning and milling of the restoration provides high precision and passive fit, therefore especially in edentulous situations a screw-retained construction is nowadays the option of choice.
Especially in the esthetic zone in situations with a considerable angle between implant and restoration axis, the screw access emerging into visible surfaces of the restoration makes a cement-retained restoration the preferred option, since the screw access channel for the abutment screw will not affect the restoration design, as the restoration is cemented over the abutment.
In the posterior area, screw access channels located in functionally loaded occlusal areas, are reported to lead to a higher incidence of ceramic chipping. Cement-retained restorations have the advantage, that the restoration is not compromised by the screw access channel, and occlusal loads can be better distributed.
Disadvantages and limitations
Subgingival excess cement has been reported as a major cause of peri-implant tissue inflammation. Adequate cementation protocols and procedures should be selected and performed in a way to avoid formation of unnecessary excess cement and ensure complete removal of cement remnants (for example placing retraction cords in the sulcus, application of a controlled amount of cement used etc.). Keeping the crown margins at an epigingival level limits flow of excess cement into the sulcus and facilitates removal of excess cements. This is especially critical in the proximal area. Ideally, customized CAD/CAM fabricated abutments are used, to enable design of the crown margin to follow the gingival profile.
For repair or maintenance usually the restoration cannot be removed from the abutments without damage, unless a temporary cement has been applied.
Cementation materials
Depending on abutment material, size and design (retention/wall angles) various cementation materials, ranging from temporary cements to adhesive resin cements, are used.
With retentive abutment designs conventional cementation protocols with zinc-phosphate or glass-ionomer cements are successfully used.
Literature describes also use of temporary cements in such situations, to allow retrieval of the restoration for repair and maintenance. However, retention with temporary cements can be unpredictable with the restoration being retained too strongly despite the cement's properties as a temporary one, or becoming loose prematurely. Temporary cements are not indicated for cementing ceramic frameworks. For a retentive abutment design, an abutment angle of 6° and abutment length of min. 5 mm is recommended. With abutment lengths below 4 mm, screw retention is recommended.
Due to the high difficulty to remove remnants of resin cements and adhesive resin cements, even more in posterior implant sites with difficult access, this type of cement is not recommended for cementation of multiple-unit restorations.