-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
Screw-retained restorations, overview
Key points
- Screw-retained design of implant-based restorations allows for easy and nondestructive retrievability of the restoration for maintenance or repair procedures
- Screw-channel orientation and access position can be adjusted through the use of Mult-unit abutments or angulated screw channel systems
- Providing the option to abandon cementation procedures and their risk of subgingival cement excess, a screw-retained design is a contribution towards healthy peri-implant tissues
Indication and principle considerations
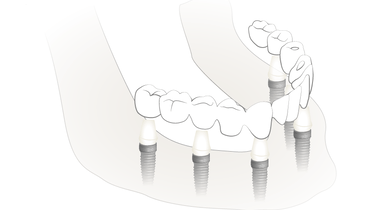
Screw-retained restorations are designed to be screwed either directly onto the implant or onto a screw-retained abutment positioned on the implant (Multi-unit Abutment). Screw-retained restorations represent a secure and easy way to maintain a prosthetic restoration.

Advantages and limitations
By simply unscrewing the restoration, adaptations, repairs and maintenance of the restorations can be performed without damaging the suprastructure. Peri-implant tissue inflammation can be treated more efficiently after removal of the supra-structure. Subgingival cement remnants are a main factor for peri-implant tissue inflammation; therefore screw-retained constructions contribute to keeping the peri-implant tissues healthy.
Use of angulated abutments enables an adequate parallelization. In the posterior zone this facilitates and enables the common insertion path for multi-unit, long-span, cross-arch restorations.
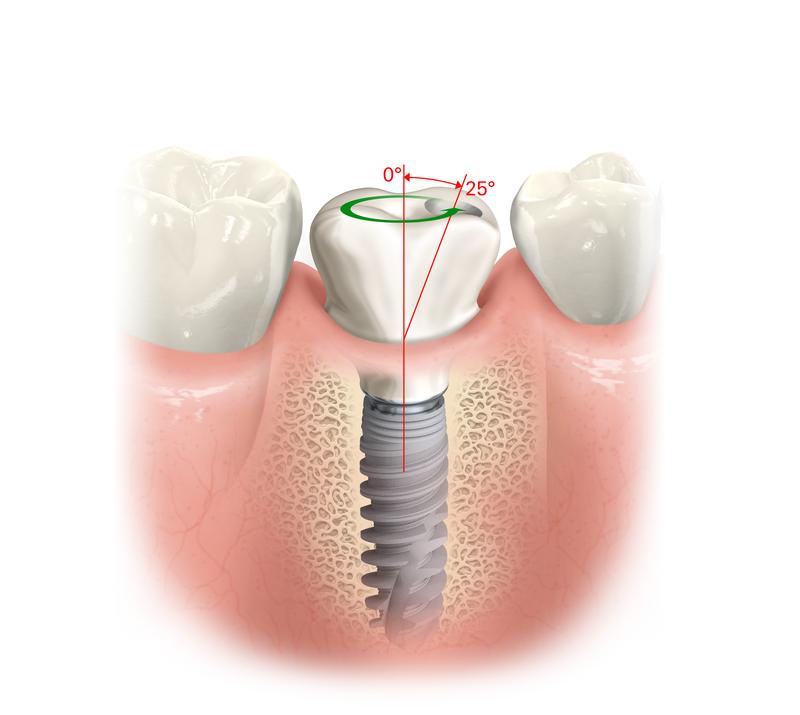
Screw-channel orientation and access position can be a challenge especially in the esthetic zone. Since the screw channel is directed in extension of the implant axis, the access opening sometimes lies on the facial, visible side of the restoration. Suitable adaptation of the screw axis onto the palatal side can be achieved by means of angulated abutments (for example Multi-unit Abutments 17° or 30°) or angulated screw channel systems with a gimballed screw/screw-driver construction, allowing an angulation of the screw channel and screw-driver axis of up to 25°. In situations, when implants are not placed deeply, please consider, that the abutment may become exposed and be visible supragingivally.
Abutment materials and design
Screw-retained abutments (Multi-unit abutments) are made from surgical grade titanium alloy. They provide a non-engaging design and low height to flexibly accommodate also low height restorations for example for limited interarch spaces. Low conus angles provide tolerance with regards to the insertion path angles. This way, differences in angulation between Multi-unit abutments and implants of up tp 40° can be compensated without using an angulated abutment.

Framework materials and design
Screw-retained frameworks can be made from titanium, Co-Cr base alloys and zirconia. CAD/CAM scanning and milling of the frameworks is the option of choice, due to its high precision (reaching 20 - 30 µm) and passive fit, which is important especially for screw-retained constructions. Considering the poor precision of casted frameworks, precious alloys loose acceptance and relevance from both a technical procedure and cost standpoint.
Titanium frameworks are usually veneered with acrylic or ceramic veneering materials, zirconia frameworks with feldspathic ceramics. Alternatively the restoration can be designed in full contour zirconia.

Complications
The most common complication in implant restorations is chipping of the veneering. Literature reports chipping rates of up to 50 %. Therefore the easy retrievability of screw-retained restorations is a major advantage. Due to high precision of modern frameworks, loosening and fracturing of the abutment screw is less frequent today and can be solved by retightening or replacing the screw.