-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
CT
Key points
- Spiral multislice CT yields the best image quality
- Supplementary panoramic and intra-oral radiographs unnecessary
- Quantitative CT allows bone density measurements
- Measurement errors must be accommodated during treatment planning
CT - Introduction
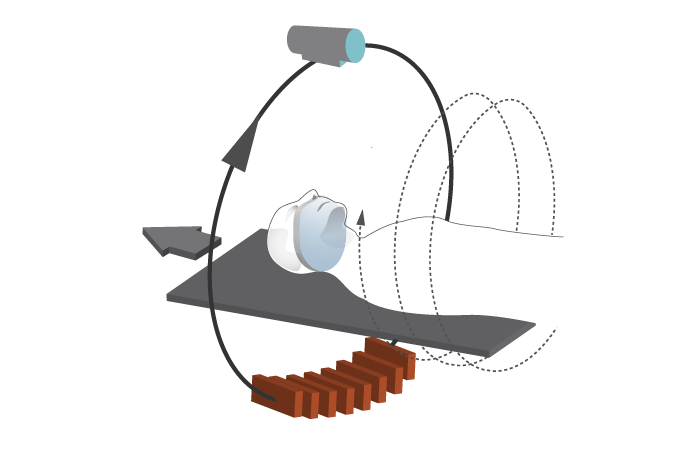
Tomography represents 2-D images of a slice through an object. Computerized tomography (CT) can produce virtual slices and conventional CTs take slice by slice and the machine stops and moves in between slices. Spiral/helical CTs are continuous scans in a spiral fashion yielding quicker and contiguous images.
There are 64 multislice scanners available that realise a resolution of < 0.5 mm and there are specific software programs for oral and maxillary image reformatting to improve the efficiency and applicability of CT imaging. The "A" in CAT refers to the axial plane although other planes, such as coronal or sagital, can be acquired.
Anatomical distances and bone volume/density calculation
Distances to the mandibular canal, overall bone height and bone width are all subject to measurement errors. Overestimations ≤ 1.1 mm, underestimations ≤1.4 mm. Therefore, these maximal values must be taken into account (“safety zone”) during treatment planning for osteotomy preparation and implant positioning.
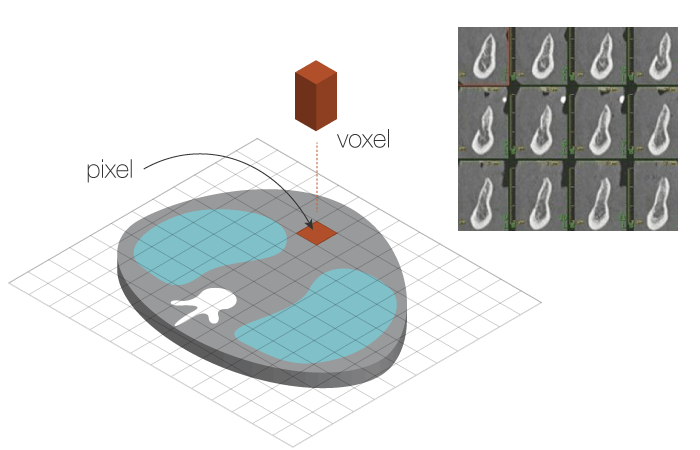
The digital data resulting from a CT scan is composed of pixels and voxels and are displayed as 3-D cross-sectional pictures. As a result, bone volume and density can be calculated.
Densities calculated from CTs are expressed in Hounsfield units (HU) and are listed below for different tissue types and maxillo-mandibular sites.
- Air = -1000
- Fat = - 80 to -100
- Water = 0
- Soft tissues = 10 to 80
- Bone = 400 to 3000.
- Maxillary cortical bone = 800 - 950
- Maxillary tuberosity cortical bone = 450 – 615
- Mandibular cortical bone = 800 - 1600
- Mandibular alveolar bone = 1300
- Mandibular basal bone = 1500.
Quantitative CT (QCT) involves the insertion of a calibration standard with the scanned body to convert HU to bone mineral density values. Sensitivity 3 – 4 x > than single-photon absorptiometry and 2 x > than dual-photon absorptiometry. Precision is lower than for the latter.



