-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
CBCT
Key points
- CBCT offers decreased irradiation dose vs spiral CT scan
- Radiation dose dependent on mA and exposure time; not on voxel size
- Dimensional accuracy has been proven to be high
- Different hardwares offer variety of fields of view (such as 4 x 4 to 15 x 20 cm) according to the clinical indication
- Both 2D and 3D images can be obtained
- Hounsfield unit measurements not as reliable as on spiral CT
- Integrating a planned or existing prosthetic device in the images is unvaluable for treatment planning
CBCT Considerations
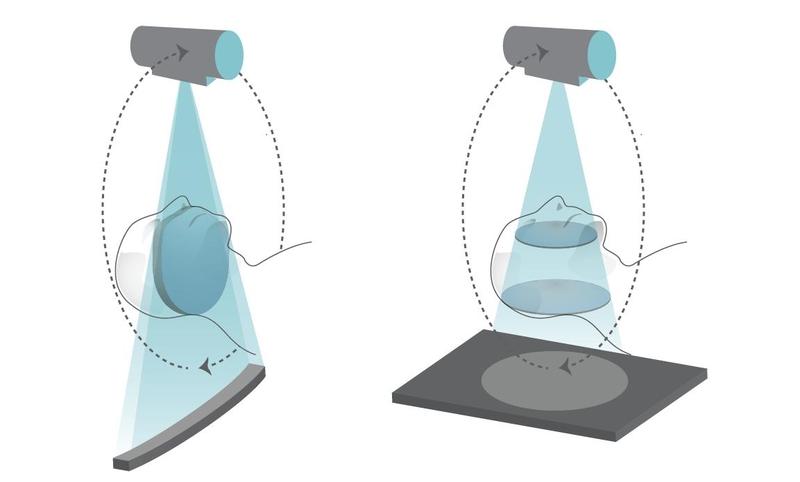
- Radiation source collimated at its source and then diverges into a fan shape to reach detectors. This results in a cone beam.
- Pixel (picture + element) is the smallest single component of a 2-D image, whereas a voxel is the smallest element in 3-D environment.
- Large fields of view (FOV) visualize both jaws and their relationship.
- Small FOVs offer detailed images of bone trabeculae and cortex.
- Grayscale values vary for specific tissues within the image and are not as reliable as in spiral CT.
- CBCT can detect clinically relevant structures which are not visible on panoramic/intra-oral radiographs, such as the incisor canal, lingual concavities and missing osseous cortex
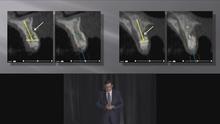
- CBCT 2-D image, showing the mesial extension of the incisor canal
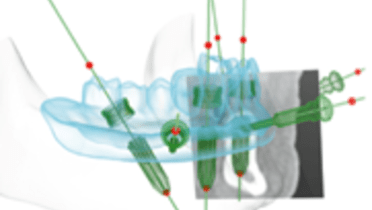
- The CBCT is essential for preoperative planning and CAD-CAM manufacturing of drill guides and/or prostheses
- Except for gray values, CBCT provides information as accurately or even better as spiral CT, with less radiation exposure and costs
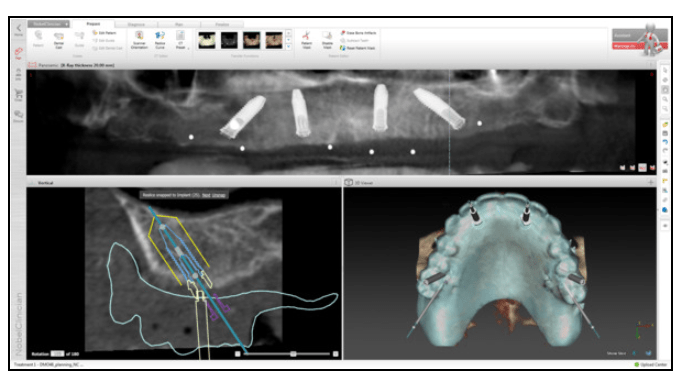
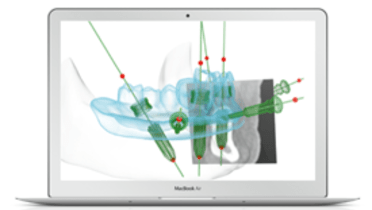
Fig 2: NobelClinician software screenshot - a CBCT is essential for preoperative planning and CAD-CAM manufacturing of drill guides and/or prostheses.
Clinical topics
Related articles
Additional resources
Additional external resources
Questions
Ask a question
Log in or sign up to continue
You have reached the limit of content accessible without log in or this content requires log in. Log in or sign up now to get unlimited access to all FOR online resources.
No payments necessary - FOR is completely free of charge.