-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
Implant-retained/supported, general
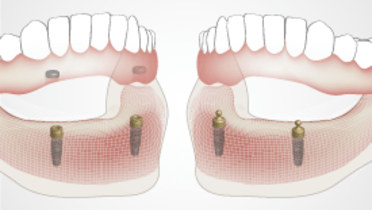
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
Implant overdenture placement
Key points
- Overdenture base fit, extensions and occlusion should be carefully evaluated and adjusted
- Overdentures may be attached to implants and immediate loading using resilient attachments and autopolymerizing resin
- Patient education and instructions are vital to ensure the desired healing, prosthesis care and management of patient expectations
Overdenture placement
Placement of a removable prosthesis requires attention to detail to cover all important clinical items such prosthesis fit, denture base extensions, esthetics, occlusion, patient comfort and post-insertion instructions. Implant overdentures may or may not be attached to the implants in the provisional phase. In addition, the clinician should communicate clearly with the patient regarding expectations with a removable prosthesis.
Denture fit and base extensions
Prosthesis fit is evaluated using disclosing media to identify areas of contact between the denture base and mucosa. Certain areas of contact should be relieved, such as over the nasopalatine fossa/incisive canal and frenuli. The primary stress bearing area of the maxilla is the crest of the alveolar ridge and an even pressure distribution bilaterally is desirable. The primary stress bearing area of the mandible is the buccal shelf and bilateral contact of the denture base with this area does not necessitate adjustment unless denture sores are observed at post-insertion appointments.
Denture base extensions must be adjusted to correct overextensions as they can lead to significant denture instability or denture sores in the case of an implant overdenture where the prosthesis does not move in response to mucosal pressure on the overextensions. Disclosing media is necessary to identify which areas of the denture base extensions to adjust as the patient is asked to recapitulate functional movements. Furthermore, denture base thickness should be adjusted to support tissues appropriately, provide a cameo surface that promotes mastication and bolus transfer, and not impinge on oral cavity space unnecessarily and annoy the tongue.
After denture fit and base extensions have been addressed, esthetics should be evaluated. Occlusion should be adjusted to achieve bilateral and stable harmonious contact in the centric position. If a balanced articulation is sought, a clinical remount is necessary for articulator mounting and extra-oral refinement.
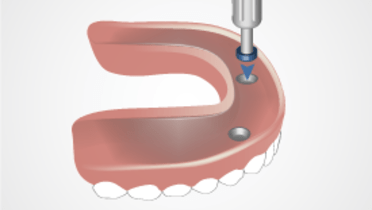
Denture connection to implants
After implants have been placed and if immediate loading is planned, the denture can be attached to the implants once overdenture resilient abutments have been seated and torqued to manufacturer recommended levels. Attachments should be related to the prosthesis intraorally using autopolymerizing resin and this should only take place after all other adjustments to the overdenture (fit, extension, occlusion) have been made. While the resin polymerizes, the patient should be asked to lightly close to position the prosthesis in centric occlusion. Once resin has polymerized, the prosthesis can be removed and excess material trimmed away. The patient should be educated how to insert and remove the prosthesis. Ideally, the patient can independently insert and remove the prosthesis before they leave the appointment.
If an overdenture is being placed on the day of implant surgery, regardless of whether the prosthesis is attached to overdenture abutments, the prosthesis may neet to be lined with a resilient liner to accommodate changes in tissue morphology caused by the surgery. The resilient liner should be replaced as needed during the healing and osseointegration phase before a definitive reline is performed or a new definitive prosthesis fabricated.
The patient is then thoroughly informed again, as a reinforcement of what would have been discussed during the treatment planning phase, of the benefits and limitations of wearing a removable prosthesis including starting with a soft diet, expectations regarding speech and mastication, and the importance of removing the prosthesis at night.