-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
Occlusion
Key points
- Occlusion comprising a broad range of form and function variations, functional aspects are considered adequate determinants of physiologic occlusion
- The masticatory system is able to functionally adapt rather well with a wide spectrum of morphological occlusal variations
- Most teeth-arrangement and occlusal concerns are readily addressed when managing edentulous patients with complete dentures
- Planning implant therapy when edentulous arch size discrepancies are present demands scrupulous clinical analysis to ensure optimal occlusion and esthetic outcomes
Occlusion - introduction
A universally accepted definition of ideal occlusion has been elusive. This is because an ideal occlusion can only be defined in broad terms of a physiological range of form and function. Functional aspects of occlusion, rather than specific anatomical teeth relations and locations, are now regarded as appropriate determinants of a physiologic occlusion given the broad context of expected human variability. This is also necessitated by the considerable range of encountered and described anatomical and dental variations that only infrequently predispose to masticatory dysfunction. These variations, unless characterized by severe discrepancies in dental arch size, morphology and teeth alignment, rarely require treatment. The masticatory system’s functional adaptability copes well with a wide spectrum of morphological departures from so-called ‘normal’ occlusions.
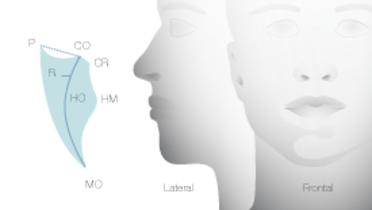
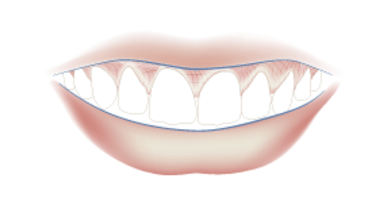
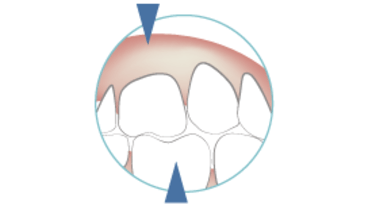
Occlusion and facial appearance
Nonetheless, the dentition plays an unquestionable role in one’s facial appearance since its form, position and arch relationships can enhance or detract from anyone’s appearance. These variants comprise most individuals’ subjective esthetic perceptions, and are influenced by cultural and social determinants in the context of age, gender, overall facial features and even personality considerations.
Consequently, matters such as different degrees of overbite and overjet, or arch form and dental-lip relationships, may be perceived as compelling reason(s) for seeking corrective changes of occlusion via orthodontic or prosthodontic treatment; and less frequently by orthognathic surgical correction.
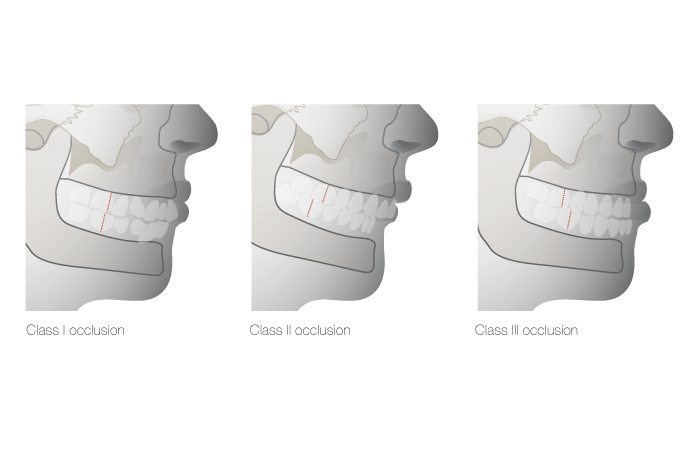
Occlusion and implant therapy
Most teeth-arrangement and occlusal concerns are readily addressed when managing edentulous patients with complete dentures. However, planning implant therapy when edentulous arch size discrepancies are present – so-called Angle Class II division 1 and Class III jaw morphologies - demands scrupulous analysis of articulated diagnostic casts to harmonize surgical and prosthodontic protocols required to achieve best possible functional and esthetic occlusion. Overdentures on implants may more easily deal with such arch size and occlusal discrepancies than fixed prostheses. Selected implant angulation, the use of angulated abutments and a bar design to 'fix' an overlying overdenture, may also offer increased design versatility.