-
0
Patient Assessment
- 0.1 Patient Demand
- 0.2 Anatomical location
-
0.3
Patient History
- 2.1 General patient history
- 2.2 Local history
-
0.4
Risk Assessment
- 3.1 Risk Assessment Overview
- 3.2 Age
- 3.3 Patient Compliance
- 3.4 Smoking
- 3.5 Drug Abuse
- 3.6 Recreational Drug and Alcohol Abuse
- 3.7 Condition of Natural Teeth
- 3.8 Parafunctions
- 3.9 Diabetes
- 3.10 Anticoagulants
- 3.11 Osteoporosis
- 3.12 Bisphosphonates
- 3.13 MRONJ
- 3.14 Steroids
- 3.15 Radiotherapy
- 3.16 Risk factors
-
1
Diagnostics
-
2
Treatment Options
-
2.1
Treatment planning
- 0.1 Non-implant based treatment options
- 0.2 Treatment planning conventional, model based, non-guided, semi-guided
- 0.3 Digital treatment planning
- 0.4 NobelClinician and digital workflow
- 0.5 Implant position considerations overview
- 0.6 Soft tissue condition and morphology
- 0.7 Site development, soft tissue management
- 0.8 Hard tissue and bone quality
- 0.9 Site development, hard tissue management
- 0.10 Time to function
- 0.11 Submerged vs non-submerged
- 0.12 Healed or fresh extraction socket
- 0.13 Screw-retained vs. cement-retained
- 0.14 Angulated Screw Channel system (ASC)
- 2.2 Treatment options esthetic zone
- 2.3 Treatment options posterior zone
- 2.4 Comprehensive treatment concepts
-
2.1
Treatment planning
-
3
Treatment Procedures
-
3.1
Treatment procedures general considerations
- 0.1 Anesthesia
- 0.2 peri-operative care
- 0.3 Flap- or flapless
- 0.4 Non-guided protocol
- 0.5 Semi-guided protocol
- 0.6 Guided protocol overview
- 0.7 Guided protocol NobelGuide
- 0.8 Parallel implant placement considerations
- 0.9 Tapered implant placement considerations
- 0.10 3D implant position
- 0.11 Implant insertion torque
- 0.12 Intra-operative complications
- 0.13 Impression procedures, digital impressions, intraoral scanning
- 3.2 Treatment procedures esthetic zone surgical
- 3.3 Treatment procedures esthetic zone prosthetic
- 3.4 Treatment procedures posterior zone surgical
- 3.5 Treatment procedures posterior zone prosthetic
-
3.1
Treatment procedures general considerations
-
4
Aftercare
Incision and wound closure
Key points
- Incision is an important point to avoid to damage anatomical structures and to obtain a perfect wound closure.
- Perform very precise incisions and carefully flap elevation.
One should have adequate knowledge of regional anatomy and treatment plan before making an incision. Atraumatic management of the soft tissues favors rapid and uncomplicated healing.
Incisions
Flap design and surgical exposure should be planned before initial incision is made. When making an incision, the operator should start posteriorly, working towards the front of the flap and it must be large enough to allow the surgeon to visualize the ridge and eventually the crest defects. Small flap causes difficulty for the surgeon and tension on the flap, resulting in excessive tissue trauma. For sulcular incisions, the blade is placed vertically into the gingival sulcus, following the shape of the tooth, keeping the sharp edge of the blade against the tooth surface to prevent unnecessary damage to gingiva. The incision can be crestal or at a distance in the labial fold. Presence of keratinized tissue both labially and palatally should ideally be achieved.
Flap reflection and protection
Flap reflection begins with the papillae. These should be turned out and separated from the underlying bone with the small triangular periosteal elevator, keeping the smooth surface towards soft tissue. Firm controlled small push will separate the papillae atraumatically.. After reflecting the papillae, the attached gingival is separated keeping the sharp edge of the periosteal elevator firmly on the bone, this is often hardest part of the flap reflection, and care must be taken to ensure the soft tissues are not put under undue tension. Then instrument is pushed downwards and backwards to complete the reflection.
Repositioning and suturing
The flap can also be replaced to a new position like in buccal advancement flap and sutures should be carefully placed to perform a complete wound closure, 4/0 to 6/0 sutures are ;used to avoid scars.
Anatomical consideration
Anatomical structures that must be taken into consideration when designing a flap are explained according to the area of flap placement.
Mandible
There are two main nerves which should be considered when planning a flap in the mandible:
Mental nerve
Radiographic image of the mental foramen prior to surgery to ensure the position is imperative. When making a flap in this region the anterior relieving incision should be placed mesial to the first premolar. The nerve lies within the buccal soft tissues and therefore will be retracted intact with the flap. Care must be taken during the procedure not to cause crush injury to the nerve by excessive pressure with the flap retractor.
Lingual nerve
In the third molar region, it is only covered by a thin layer of mucous membrane. When making incisions in the posterior mandible, especially in this region, all incisions should be made buccally to prevent severing the nerve. Lingual flap can be kept intact during third molar surgery to prevent lingual nerve injury.
Maxilla
The hard palate is innervated by the greater palatine nerve, with which the greater palatine vessels run. The vast majority of palatal surgeries are done using an envelope flap around the necks of the teeth, the neurovascular bundle are reflected with the flap without much difficulty. If vertical relieving incision is required for access, then this must be done at the anterior end of the flap, as posterior relieving incision will severe the greater palatine vessel causing brisk bleeding.
Figure 1 Figure 2 Sinus lift & GBR procedures
Figure 3 Figure 4 Figure 5 Full thickness flap at implant placement
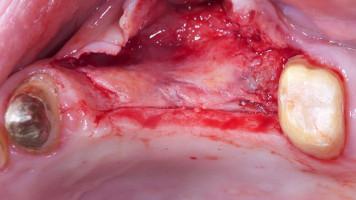
Figure 6: Partial thickness flap at II surgery
Figure 7: Mandibular full thickness flap before implant placement and GBR Figure 8: Partial thickness flap at II surgery














