-
0
Patient Assessment
- 0.1 Patient Demand
- 0.2 Anatomical location
-
0.3
Patient History
- 2.1 General patient history
- 2.2 Local history
-
0.4
Risk Assessment
- 3.1 Risk Assessment Overview
- 3.2 Age
- 3.3 Patient Compliance
- 3.4 Smoking
- 3.5 Drug Abuse
- 3.6 Recreational Drug and Alcohol Abuse
- 3.7 Condition of Natural Teeth
- 3.8 Parafunctions
- 3.9 Diabetes
- 3.10 Anticoagulants
- 3.11 Osteoporosis
- 3.12 Bisphosphonates
- 3.13 MRONJ
- 3.14 Steroids
- 3.15 Radiotherapy
- 3.16 Risk factors
-
1
Diagnostics
-
2
Treatment Options
-
2.1
Treatment planning
- 0.1 Non-implant based treatment options
- 0.2 Treatment planning conventional, model based, non-guided, semi-guided
- 0.3 Digital treatment planning
- 0.4 NobelClinician and digital workflow
- 0.5 Implant position considerations overview
- 0.6 Soft tissue condition and morphology
- 0.7 Site development, soft tissue management
- 0.8 Hard tissue and bone quality
- 0.9 Site development, hard tissue management
- 0.10 Time to function
- 0.11 Submerged vs non-submerged
- 0.12 Healed or fresh extraction socket
- 0.13 Screw-retained vs. cement-retained
- 0.14 Angulated Screw Channel system (ASC)
- 2.2 Treatment options esthetic zone
- 2.3 Treatment options posterior zone
- 2.4 Comprehensive treatment concepts
-
2.1
Treatment planning
-
3
Treatment Procedures
-
3.1
Treatment procedures general considerations
- 0.1 Anesthesia
- 0.2 peri-operative care
- 0.3 Flap- or flapless
- 0.4 Non-guided protocol
- 0.5 Semi-guided protocol
- 0.6 Guided protocol overview
- 0.7 Guided protocol NobelGuide
- 0.8 Parallel implant placement considerations
- 0.9 Tapered implant placement considerations
- 0.10 3D implant position
- 0.11 Implant insertion torque
- 0.12 Intra-operative complications
- 0.13 Impression procedures, digital impressions, intraoral scanning
- 3.2 Treatment procedures esthetic zone surgical
- 3.3 Treatment procedures esthetic zone prosthetic
- 3.4 Treatment procedures posterior zone surgical
- 3.5 Treatment procedures posterior zone prosthetic
-
3.1
Treatment procedures general considerations
-
4
Aftercare
Impression options and protocols, posterior zone
Key points
- The restorative dentist has a myriad of impression options in the posterior zone.
- The choices in the material are multiple.
- The options for digital impression procedures are increasing.
The first choice the restorative dentist must make is whether the impression will be performed at the abutment or fixture level. This depends upon a number factors, some of which are, position of the implant relative to adjacent structures (teeth or implants) depth of soft tissue, morphology of the soft tissue, restorative space, posterior inter-occlusal space and dentist preference.
Fixture (Implant) Level Impression
This requires open or closed tray impression copings. Depending on the amount of space one has for material, tray and impression coping this may be challenging. The critical part of this impression is the capturing the angulation, depth and rotation of the implant insuring the final restoration is oriented correctly in all directions.
Abutment Level Impression
If the impression is to be at the abutment level this can be a (cement retained option) custom or stock abutment. In the screw retained option the utilization of a custom or stock angulated abutment (allows for a screw from the lingual surface) or the angulated screw channel approach (ASC). Of note the accuracy of the final impression is dependent on the complete seating any of the above components and verification via radiograph. The literature is conclusive that all procedures have some form inaccuracy that must be expected.
Material choice is again dependent upon the preferences of the restorative dentist. The material should be one that would be utilized in conventional fixed dental prosthesis construction (polyethers, polyvinylsiloxanes, putty – wash combinations, etc). The literature is also conclusive on this subject, impression materials of the previously mentioned categories are all suitable with no one product demonstrable better.
With the increasing use of the digital realm it is possible thru the use of scan bodies or specific healing abutments to capture the orientation of the implant architecture without the use of impression material. This approach is becoming increasingly more popular and potentially will reduce costs and reduce treatment times. One consideration here is the size of the intra-oral scanner, as this may limit the ability to capture the image if space is limited.
Figure 1: Healing abutment in place (not platform switched). Bone loss is down to the first thread Figure 2: Demonstrates good implant placement for screw retention and the design of occlusal porcelain so as to minimize the metal show through Figure 3: Demonstrates platform switch of the abutment, notice the retention of the osseous tissue up to and above the platform
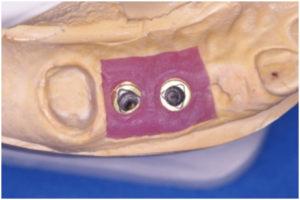
Figure 4: Tri-lobe






